| |
IV./2.3.: Subarachnoid haemorrhage
IV./2.3.1.: Pathogenesis of the subarachnoid heamorrhage (haemorrhagia subarachnoidealis).
The subarachnoid space is the third, real physical space among the 5 intracranial spaces (intracranialis cavities – epidural, subdural, subarachnoid, intraparenchymal, and intraventricular – [1A-E. Macropgraphs]), in which blood may get into due to various reasons.
|

Look into the pictures!
|

Macrograph 1: The five intracranial cavities are demonstrated by the macroscopic picture of haemorrhages that are present in the cavities: epidural (A.), subdural (B.), subarachnoid (C.), intraparenchymal (D.), intraventricular (E.) haemorrhages. (From the image-archive of the Semmelweis University, 2nd Department of Pathology–collection of Attila Kovács )
|

Macropgraph 2:Subarachnoid haemorrhage (SAH) developed dominantly in the area of the scala posterior, and in the ventral surface of the brainstem, infiltrating the cerebellar haemispheres and floods the chiamatic cistern rostrally either. The bleeding is due to the rupture of a sacciform aneurysm in the area of the bifurcation of the basilar artery. (A favor of Péter Molnár; University of Debrecen, Medical and Health Sciences Center, Department of Pathology)
|

Drawing 1: Subarachnoid haemorrhage in the midline of the brain (median-sagittal section). The haemorrhage primarily went under the pia mater, secondly got into the fourth ventricule, and then it ascended to the level of the aqueductus cerebri.
|

Macropgraph 3A-B.: A: A giant aneurysm of the right posterior communicans artery. Interestingly, this saccular dilatation (sacciform aneurysm) had not caused any clincial symptom, it was only an incidental finding during the autopsy. The cut that can be seen on the rigid, thick, hyalinic wall is only an artifact. The vertebral arteries and the basilar artery show a snake-like dilatation (cirsoid aneurysm). (A favor of Péter Molnár; University of Debrecen, Medical and Health Sciences Center, Department of Pathology). B: The aneurysm of the left a. carotis interna that can be seen on this picture was also an incidental finding during autopsy, meaning that it had remained „silent” during the life course of the patient, and showed the typical apperarance of berry aneurysms. (From the image-archive of the Semmelweis University, 2nd Department of Pathology–collection of Attila Kovács)
|
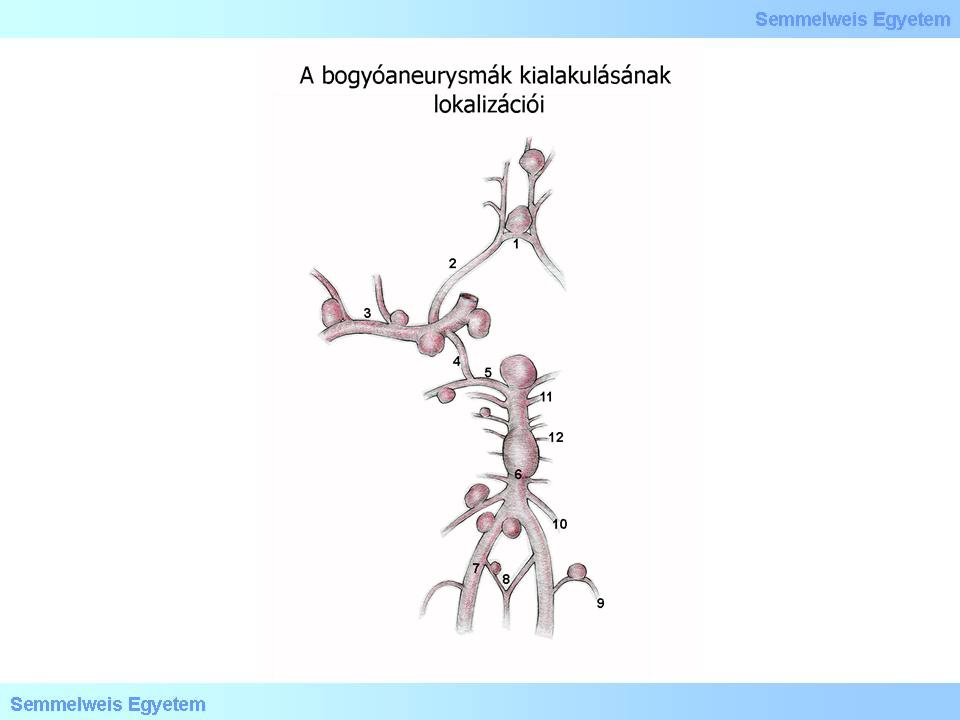
Drawing 2: Berry aneurysm may develop in many parts of the cerebral vascular system, especially at bifurcations.
|
|
 |
The berry aneurysm (Beerenaneurysma – in German) is a local dilatation of the basal cerebral arterial system, with typical appearance, which makes it one of the saccular aneurysms (sacciform aneurysm).
Prevalence rates of the most frequent causes:
-
- Rupture of berry aneurysms of the basal cerebral arteries: 75%;
-
- vascular malformation (AVM), cavernous malformation ("cavernoma"): 5-10%;
-
- infective, fusiform aneurysma, and congophil amyloid angiopathia: 5-6%;
-
- idiopathic (unknown origin): kb. 10%.
|

Look into the pictures!
|

Macropgraphs 4A-B: Relatively circumstantial SAH in the right fronto-parietal region (A.).The destructive haemorrhage that infiltrated the subarachnoidal space has been revealed by the slicing of the brain (B.). (A favor of Péter Molnár; University of Debrecen, Medical and Health Sciences Center, Department of Pathology)
|
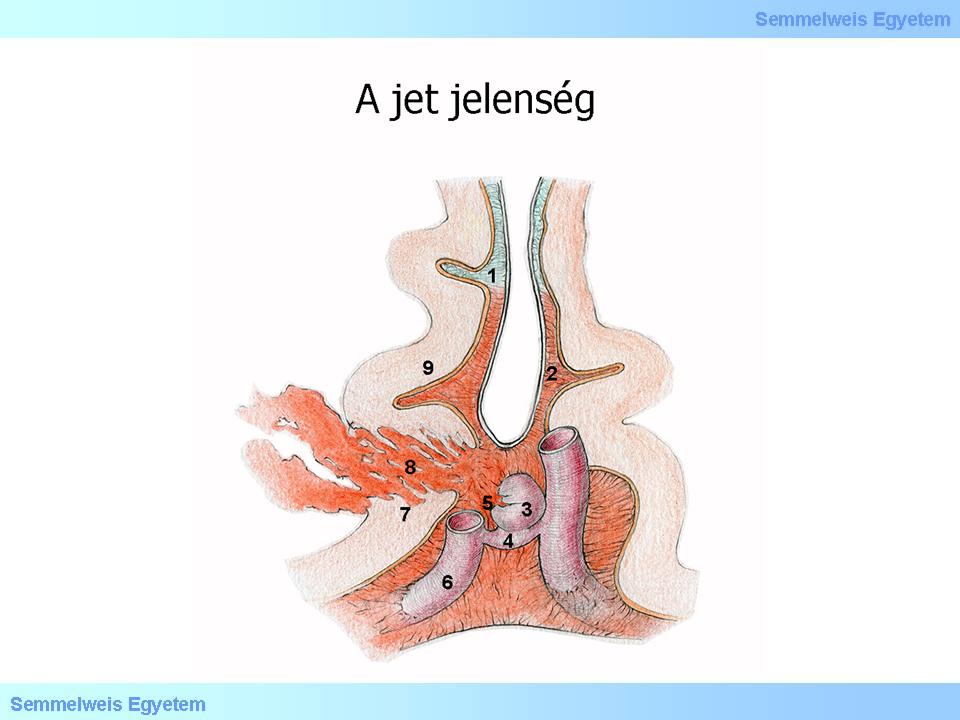
3. rajz: A drill-like blood stream ejaculates from the rupture of the blood vessel (berry aneurysm) that causes a tunnel-like brain tissue damage (jet-phenomena).
|
Berry- or saccular aneurysms are typical in the anterior intracranial circulation.
Prevalence of the isolated, non-traumatic subarachnoid haemorrhage is 6-17/100 000 inhabitants.
IV./2.3.2.: Course
An ictal start with sudden, sharp, ripping headache, disturbing complete well-being, is typical for SAH. Generally it is accompanied by rapid loss of consciousness. The symptomatology mirrors meningism and increased intracranial pressure: headache, neck stiffness, drifting eye. Blood in the lumbal liquor is pathognomic; the indication for the punction is the due of a specialised neurologist, and the liquor containing blood needs to be differentiated from the contaminated samples containing artifact!
|
Comment
|
The clinical picture corresponds to that of stroke. The blood pressure out-thrust after cocain consumption („cocain flash”) is a pathologic situation. Hypertonia (morbus hypertonicus), hyperthyreosis, hypertensive crises caused by neuroendocrin (used to be called: carcinoid) tumors are also risk factors.
Mortality is high, 16-24% of all deaths due to cerebrovascular reason is caused by subarachnoid haemorrhage.
|

Look into the pictures!
|
Title: Macropgraph 5A-D: A possible surgical treatment for subarachnoid haemorrhage is the strangulation of the origin of its saccular dilatation (the so called neck of the aneurysm („clipping” ). Beside this, placing a „self-opening”coil (coil ) into the cavity of the aneurysm is also more and more frequently applied technique, taken from interventional neuroradiology, where this technique has already been settled. With the application of the coil, it functions as a local core for stimulating clotting. The thrombus that develops then fills out the aneurysm sack and tamponades the aneurysm from inside, including that weak structural point based on which the aneurysm developed in the first place.
A: Clip on the neck of the aneurysm B: Coil-treatment. The aneurysm had developed in the first part of the medial cerebral artery, and then ruptured. After this the treatment has taken place, a spiral has been placed into the dilated part of the artery: at the bottom of the picture, the „coil” sinking into the haematoma can be observed. In the left Sylvian-fissure, blackish-red clotted-fixated blood can be seen. Eventually, the patient died due to the extensive SAH. The subarachnoid haemorrhage got into deeper parts of the parenchyma through the Virchow-Robin spaces.. C: The removed part of the coil. D: A close picture of the aneurysm sack, after blood has been washed out. (A favor of Péter Molnár; University of Debrecen, Medical and Health Sciences Center, Department of Pathology).
|
|