| |
II./4.5.: Neuroepithelial tumours
II./4.5.1.: Pilocytic astrocytoma (WHO: grade I)
|
 |
The pilocytic astrocytoma is one of the most prevalent tumours in childhood, which is often diagnosed late due to its slow growth. The tumour occurs rarely in adulthood. The most frequent localizations of the tumour are the midline structures, such as the optic nerve, the optic chiasm, the diencephalon, the brain stem and the cerebellum.
II./4.5.2.: Low grade gliomas (LGG, WHO: grade II)
|
 |
The group of low grade gliomas includes the following tumours: astrocytoma, oligodendroglioma and mixed oligoastocytoma. The tumours occur most often in the frontal lobe; average age is around 35. Symptomatic epilepsy, which is sometimes present for years without neurological symptoms is a characteristic feature of 50-80% of cases. On CT scan LGGs usually appear as low density, non-enhancing, infiltrative, most often non-space-occupying lesions. On MRI scans LGGs are usually also non-enhancing with low signal intensity on T1-weighted and high signal intensity on T2-weighted MRI sequences.
|

Study the images, and analyze what you see!
|

1. fotó: Rad Jobb oldali temporalis low grade glioma T1 sagittalis MR képe – Balogh Attila
|
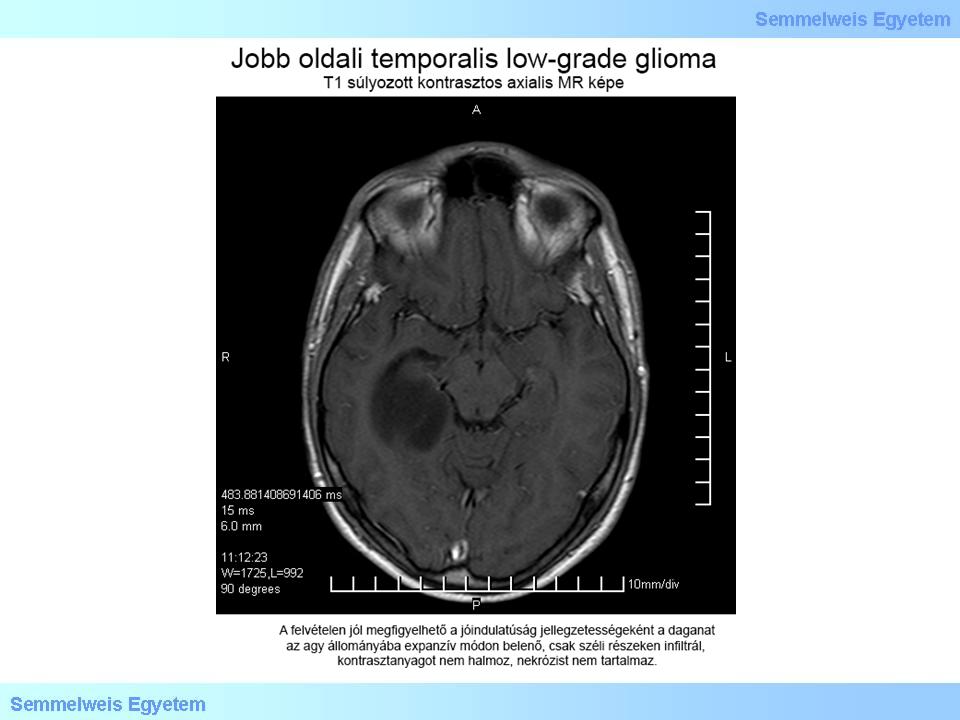
2. fotó: Jobb oldali temporalis low grade glioma T1 axialis MR képe - Balogh Attila
|
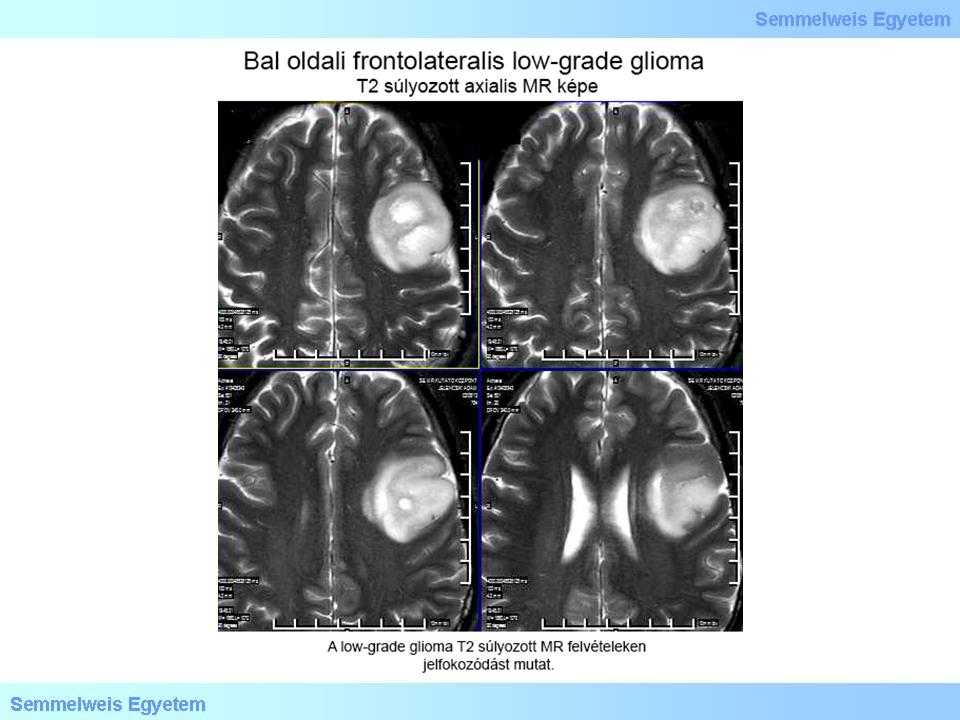
3. fotó: Bal oldali frontolateralis low-grade glioma T2 axialis MR képe – Balogh Attila
|
II./4.5.3.: Malignant glioma (WHO: grade III)
Malignant gliomas involve anaplastic astrocytoma (AA), oligodendroglioma (O) and mixed oligoastrocytoma (AO). Spontaneous dedifferentiation can be observed in as high as 50% of oligodendrogliomas and AOs. The tumours occur most frequently between the ages 35-55. CT scan shows a low or mixed density with indistinct borders, contrast enhancement, perifocal oedema and intracranial space occupation. In case of tumours with oligodendroglial components calcifications can be observed as well. On MRI scans malignant gliomas show mixed intensity with speckled enhancement. Infiltration to the surrounding tissue can be best seen on T2-weighted sequences in the form of high intensity, which exceeds the enhancing area when compared to T1-weighted sequences. Relevant prognostic factors are the age of the patient, the neurological status before surgery and the extent of surgical removal.
II./4.5.4.: Glioblastoma multiforme (WHO: grade IV)
|
 |
CT and MRI scans most frequently show an annular contrast enhancement, with hemosiderin referring to bleeding on MRI. It has been mentioned in the introduction that there are primary and secondary GBMs. Despite its histological features GBM developing from benign glioma is of better biological nature. The first therapeutic step is surgery here as well, followed by chemo-irradiation. If the surgical removal of the tumour can not be performed due to its localization (e.g.: a bilateral ’butterfly’ tumour infiltrating across the corpus callosum), or because of the neurological status and/or age of the patient, then it is necessary to perform a stereotactic biopsy for differential diagnosis (e.g.: the exclusion of an abscess).
|

Study the images!
|

4. fotó: Jobb oldali temporalis glioblastoma multiforme T1 axialis MR képe – Balogh Attila
|
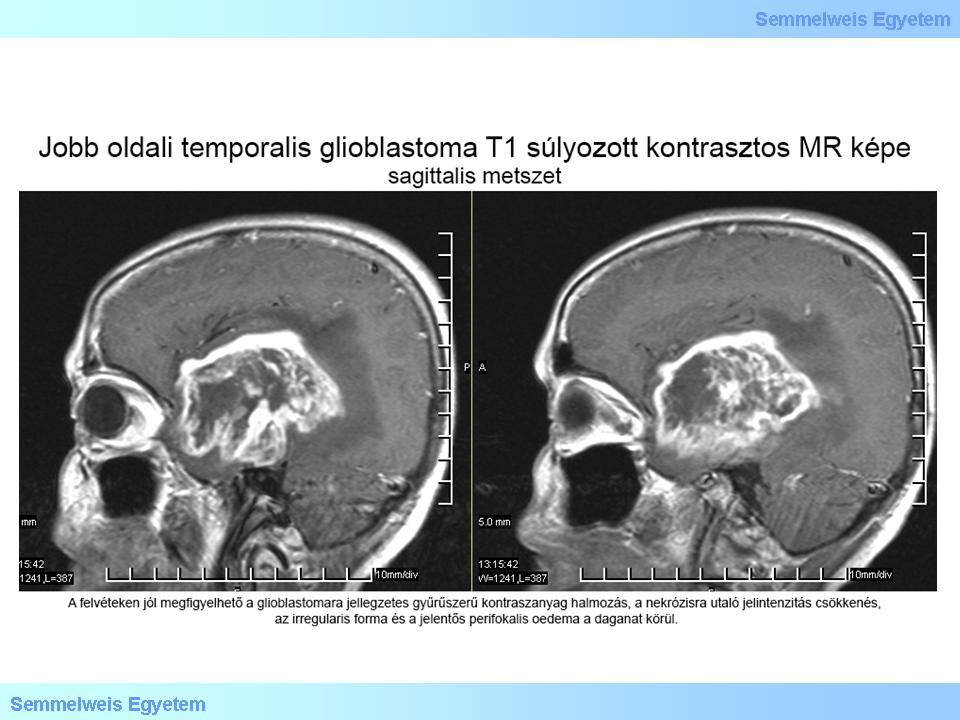
5. fotó: Jobb oldali temporalis glioblastoma multiforme T1 sagittalis MR képe – Balogh Attila
|
II./4.5.5.: Ependymoma
Ependymomas typically develop in childhood. Malignisation can occur, which could be accompanied by metastases in the nervous system. The tumour develops from the ependyma of ventricular walls and from the reminiscence of the central canal of spinal cord. Ependymomas often occur in the fourth ventricule and in the lateral ventricles. CT scan demonstrates isodense tumours, or ependymomas of mixed density tightly attached to the ventricular system with speckled contrast enhancement. A dilated supratentorial ventricular system is a common finding in case of a tumour located in the posterior cranial fossa. (7). In these cases the symptoms of ependymomas include nausea, vomiting and headache.
II./4.5.6.: Medulloblastoma (WHO: grade IV)
Medulloblastoma is a tumour of embryonic origin, which corresponds to the WHO: grade IV tumour type. This is the most prevalent childhood tumour located in the posterior cranial fossa. (6). In adulthood its typical occurrence is between 21-40 years. On CT scans medulloblastoma appears as a midline, distinct, high density tumour with strong and homogenous enhancement. On T1-weighted sequences medulloblastoma shows a low signal intensity, while on T2-weighted sequences the tumour is either hypointense, isointense, or hyperintense with a homogenous, strong enhancement. MRI scans with contrast make it possible to reveal small cortical and basal metastases. Medulloblastomas spread via liquor as well, so complex stereotactic irradiation is recommended after the surgical removal. (8) Metastases outside the nervous system (bone, lung) have been described as well. Desmoplastic medulloblastoma, which is associated with a better prognosis occurs with a higher prevalence in young adults.
|
|