| |
I./2.3.: Intraventricular haemorrhage
I./2.3.1.: Essentials of cerebral haemorrhage
|
 |
A structural damage (arterio-, arteriolosclerosis, amyloid deposition, etc.) occurs in the wall of some part of the intraparenchymal vasculature – usually a small vessel (most often a small artery or arteriole) – leading to a discontinuity in the vessel’s wall (rupture). Blood escaping with the systolic pressure damages the surrounding parenchyma. In time, localized collection of blood (cerebral hematoma) (Macropicture 1) can occur. The parenchyma can be destructed without the relative distancing of the hematoma (in both cases we are faced with space-occupying / space reduction process). The process typically starts in the basal ganglion area as a complication of high blood pressure (hypertonia, morbus hypertonicus).
The destructive brain haemorrhage – in case of deep location - can break into the ventricular system (usually the cella media region of one of the lateral ventricles is at risk) and it can partially or completely fill it as a cast (haemocephalus internus partialis seu totalis). (Macropicture 2.)
Also as a secondary process – in case of superficial location – the bleeding can break in the subarachnoidal space , mimicking subarachnoidal haemorrhage (haemocephalus externus) (Macro pictures 3 and 4)
|

Look into the pictures!
|
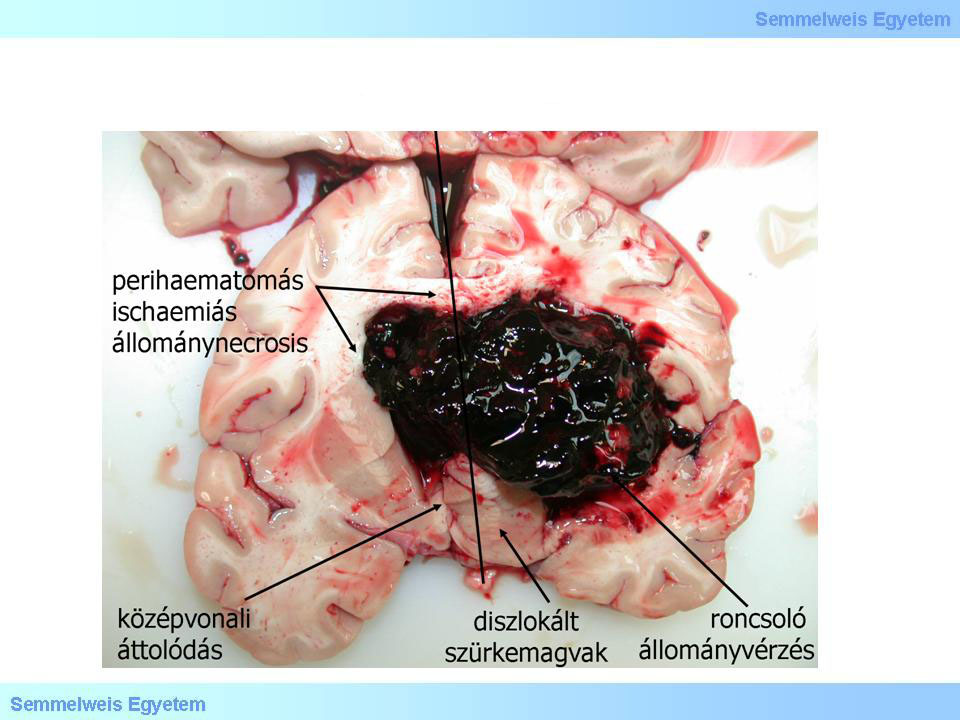
Macropicture 1: Destructive parenchymal haemorrhage which dislocated the midline structures to the opposite side with its space occupying effect. A secondary perihaematomic ischemic courtyard is formed. (Source: Semmelweis University 2nd Department of Pathology picture archives, collected by Attila Kovacs)
|
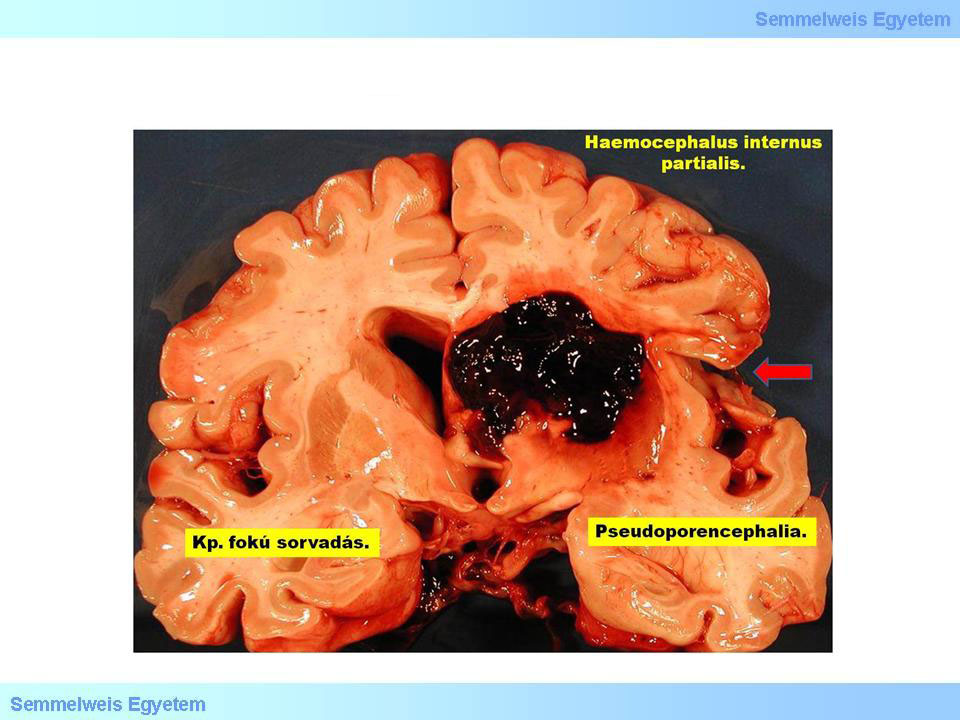
Macropicture 2: Haemocephalus internus partialis, as a consequence of the neighbouring brain parenchymal haemorrhage (Source: DEOEC Department of Pathology, courtesy of Peter Molnar)
|
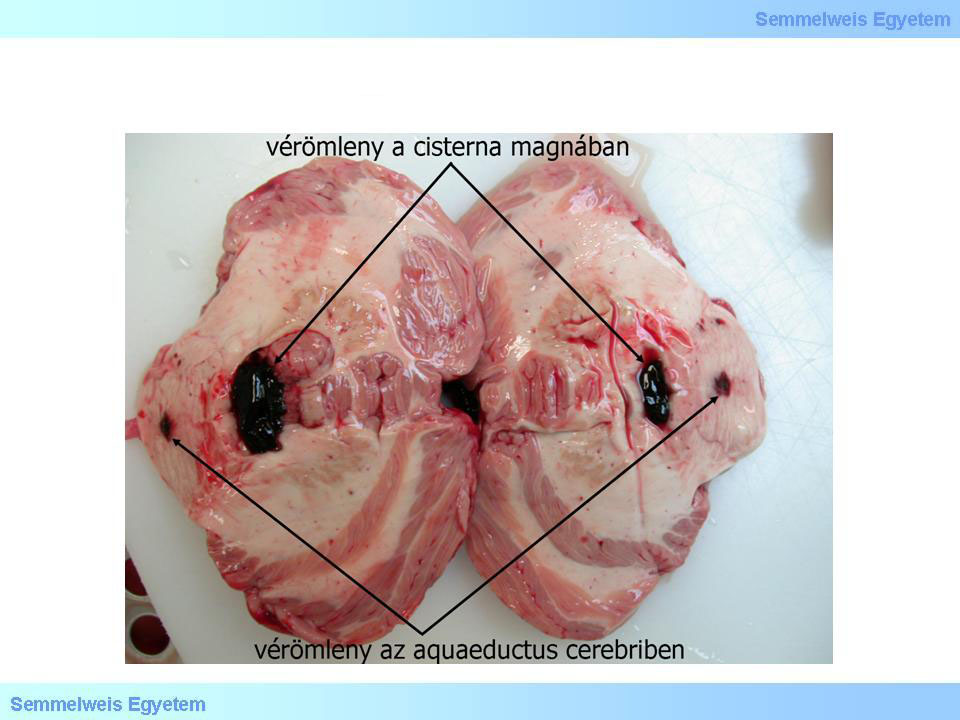
Macropicture 3: Only secondary propagation areas of an intracerebral haemorrhage can be seen here: on one hand, the spread into the ventricular system (here: aquaeductus cerebri), on the other hand the propagation from here to the cisterna magna (Source: Semmelweis University 2nd Department of Pathology picture archives, collected by Attila Kovacs)
|
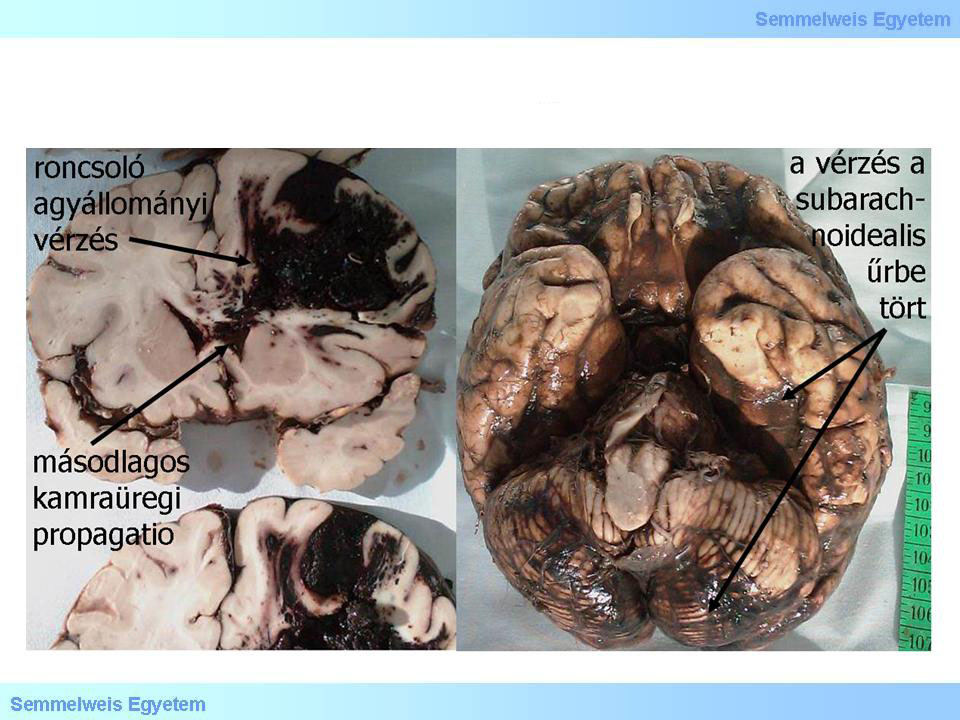
Macropicture 4: Severe hemorrhagic brain tissue damage causing extensive, direct subarachnoideal haemorrhage and ventricular haematoma. (Source: DEOEC Department of Pathology, courtesy of Peter Molnar)
|
|

Please look into the pictures carefully!
|
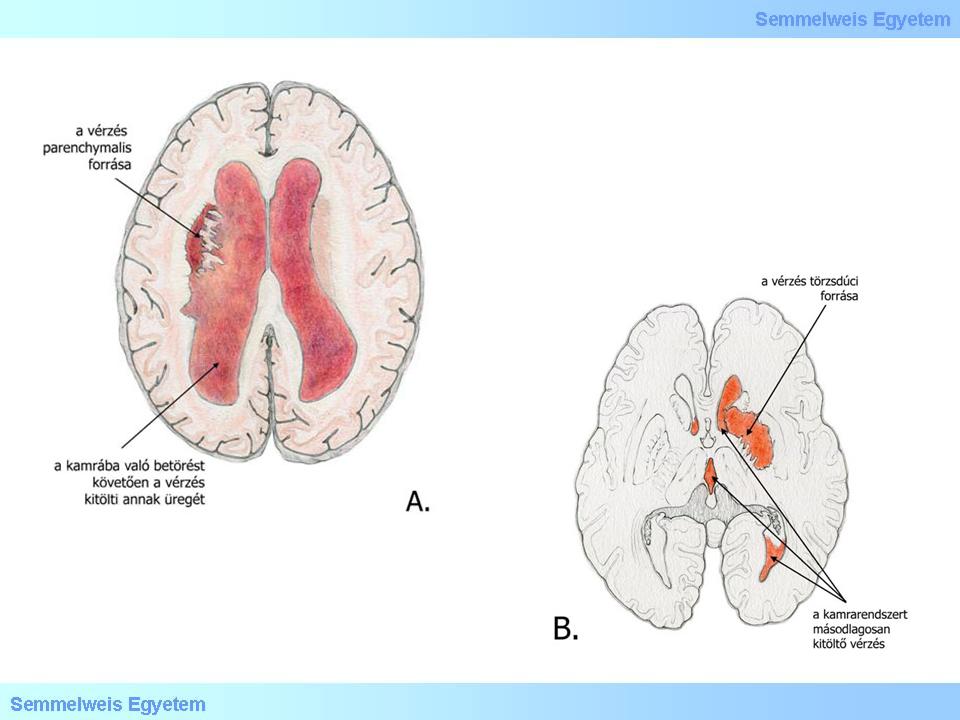
Drawings 1 A-B: Commonly deep intracerebral haemorrhages are complicated with ventricular propagation.
|
I./2.3.2.: Pathogenesis
|
 |
Segmental, localized dilatations up to 1 mm size (miliary aneurysms, Charcot-Bouchard microaneurysms) on the small (25-250 micron diameter) intraparenchymal arterioles are considered relevant in its pathogenesis, namely they could be the origin of the destructive brain haemorrhage. In hypertonic disease, small vessels can breach even without such aneurysms, as the vessel wall is destructed by hyalinosis-lipohyalinosis in benign, and fibrinoid necrosis in malignant hypertension. The damaged vessel segment typically "explodes", disappears in the haemorrhage, which makes it difficult to identify the lesion responsible for its pathogenesis.
Fresh intracerebral bleeding often demarcates, the exudate is finite in these cases. When occupying space, it is disposed for spreading dissection among the existing structures, nerve pathways, ganglia, but due to its compressive and tensile effect it also causes perihaematomal brain tissue necrosis. The insufficient blood supply (ischemia) of the areas surrounding the primarily damaged parenchyma (Macropicture 1.) and the release of paracrin, biologically active messenger molecules also has a role in its pathogenesis. With some time lag, worsening oedema aggravates the situation. The postnecrotic oedema is caused by the osmotic suction force of the disintegrating tissue, but the vasogenic component (the blood-brain barrier damage) cannot be ignored either.
I./2.3.3.: Possible anatomical localizations of the disease
|
 |
Haemorrhages above or under the cerebellar tentorium (supra- and infratentorial) can be distinguished. Supratentorial haemorrhages can be further classified based on their position according to the lobes (so-called lobar haematomas: frontal, parietal, (Macropicture 5.) temporal, occipital); or based on their deep location independent of the lobes (so-called deep – e.g. brain stem, paraventricular etc. – haemorrhage). (Neurological classifications are usually based on specific arterial branches: haemorrhages in the supply area of the a. lenticulostriata, or area of Heubner’s a. recurrens, or supply area of a. chorioidea anterior etc.)
Most of the spontaneous cerebral haemorrhages associated to hypertension are „striato-capsular” (putamen + capsula interna), male patients having this disease often have alcohol dependency as well. Hypertonic cerebral haemorrhages occur mostly (60%) in deep localizations (putamen, thalamus), less commonly in the hemispheres (20%), cerebellum, pons. The haematoma is usually monophasic, it develops within hours, but due to the high perfusion pressure caused by the increased intracranial pressure, it can keep growing for 10-12 hours. The perifocal oedema and the surrounding reactive ischemia (Macropicture 5.) both contribute to the parenchymal damage.
|

Look into the pictures!
|
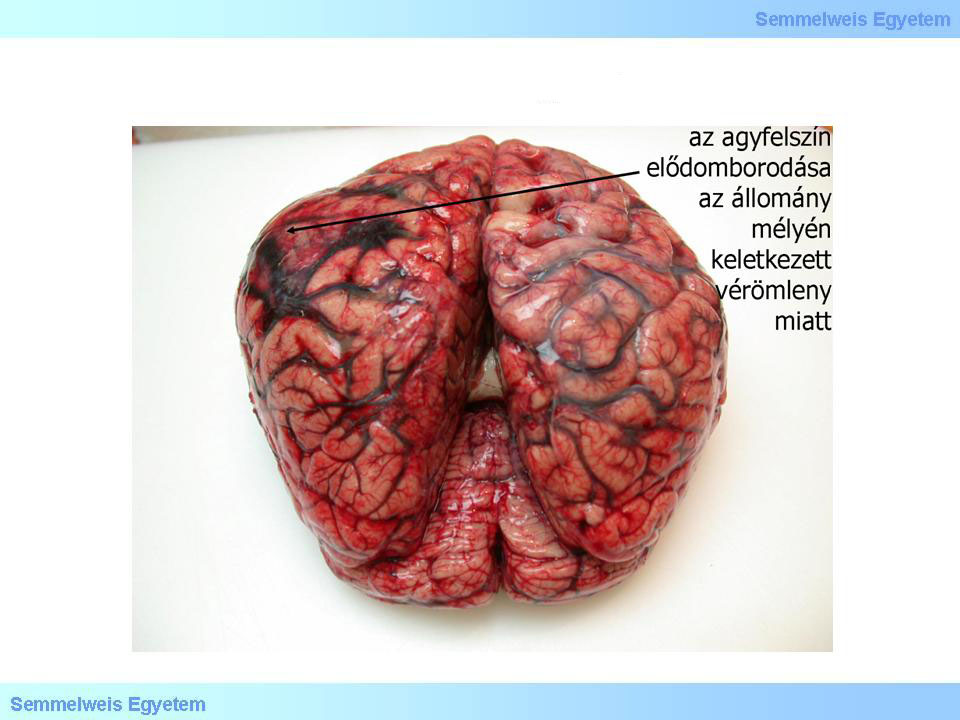
Macropicture 5: Parietal lobe haemorrhage, which bulges the neighbouring cerebral surface as a sign of space occupation. (Source: Semmelweis University 2nd Department of Pathology picture archives, collected by Attila Kovacs)
|
Drawings 2 A-D. Different locations of intracerebral haemorrhage: parietooccipital lobe haemorrhage (A); basal ganglia (deep) haemorrhage (B); intracerebellar haemorrhage (C); brain stem- pons haemorrhage (D).
I./2.3.4.Etiology
|
 |
Cerebral haemorrhages are most commonly caused by hypertonic disease. Sixtyfive-eightyfive percent of the patients suffers from hypertension to some degree. (Percentages vary with regions, countries and textbooks; this number is an average value, estimated without using specific criteria!). Hypertonic cerebral haemorrhages are commonly deeply located and disposed to spreading into the ventricles. Further causes: cerebral amyloid angiopathy (CAA – around 15-20 %), anticoagulant therapy (10%), tumours (primer tumor or metastasis – 8%), drug abuse (6%), arteriovenous malformation, „cavernoma” and aneurysms (5%). Bleeding can be also caused by moyamoya disease or venous angioma (DVA – developmental venous anomaly). In 10-15% of the cases the cause cannot be ascertained, however, excessive alcohol consumption, diabetes, coagulopathy (aspirin or heparin can cause cerebral haemorrhage!) is often detected.
|

Look into the picture!
|
6A-B. Macropictures: Herniation fissure in brain stem herniation (herniatio tonsillarum cerebelli) (Source: Semmelweis University 2nd Department of Pathology picture archives, collected by Attila Kovacs)
|
|