| |
V./2.3.: Hemispheric acute and chronic softening of the brain
V./2.3.1.: Circulation disturbances; cerebral ischaemia and hypoxia
|
 |
The cerebral circulation disturbances are accompanied by the decrease of glucose- and oxygen supply, as well as by the insufficient removal of the metabolic products. Hypoxia means the decrease in oxygen supply, while anoxia means the complete lack of oxygen.
According to the most prevalent grouping, there is
- hypoxaemic,
- stagnant, and
- histotoxic hypoxia.
|

Please look into the pictures carefully!
|

Macrographs 2A-C: A-B: The macroscopic feature of acute cerebral softening is the pulpy dissolving of the tissue in an area without sharp border. C: Over time, the necrotized area becomes more and more distinct from the living tissue in its environment. In this case, the progressive demarcation indicates the subacute phase of this infarct in the pontin too. (From the image-archive of the Semmelweis University, 2nd Department of Pathology–collection of Attila Kovács)
|

Macrograph 3: Multiple microvascular dilatation of the necrotic area, causing a reddish, pointed-dotted outlook of the affected area, is a frequently observed concomitant phenomenon of acute cerebral infarcts. The phrase applied to this, „luxury perfusion”, however, is rather a clinico-radiologic concept. It is based on the necroparalytic dilatation of the vessels traveling through the affected area. Nonetheless, this passive congestion does not go together with the improved perfusion of tissues after the ischemic insult, but it can be considered as part of the necrotic process. Borderline infarction develops in the peripheral parts of the vascularisation zones of cerebral tissue. (From the image-archive of the Semmelweis University, 2nd Department of Pathology–collection of Attila Kovács)
|

Macrograph 4: The chronic infarction is indicated by the sharp demarcation, and the formation of a pseudo-sac cavity due to the progressive colliquation and softening of the necrotized area. (From the image-archive of the Semmelweis University, 2nd Department of Pathology–collection of Attila Kovács)
|
V./2.3.2. Cerebral infarction
|
 |
An ischemia based colliquation necrosis of the brain tissue, that follows the anatomical vascularisation zones. There are multiple reasons in the background of cerebral infarction, mostly associated with the cerebral vessels, or the condition of the blood flowing in these vessels, like.:
-
angiopathies of the greater blood vessels (macroangiopathies),
-
small vessel diseases (microangiopathies),
-
coagulopathies.
|

Look into the picture carefully!
|
-
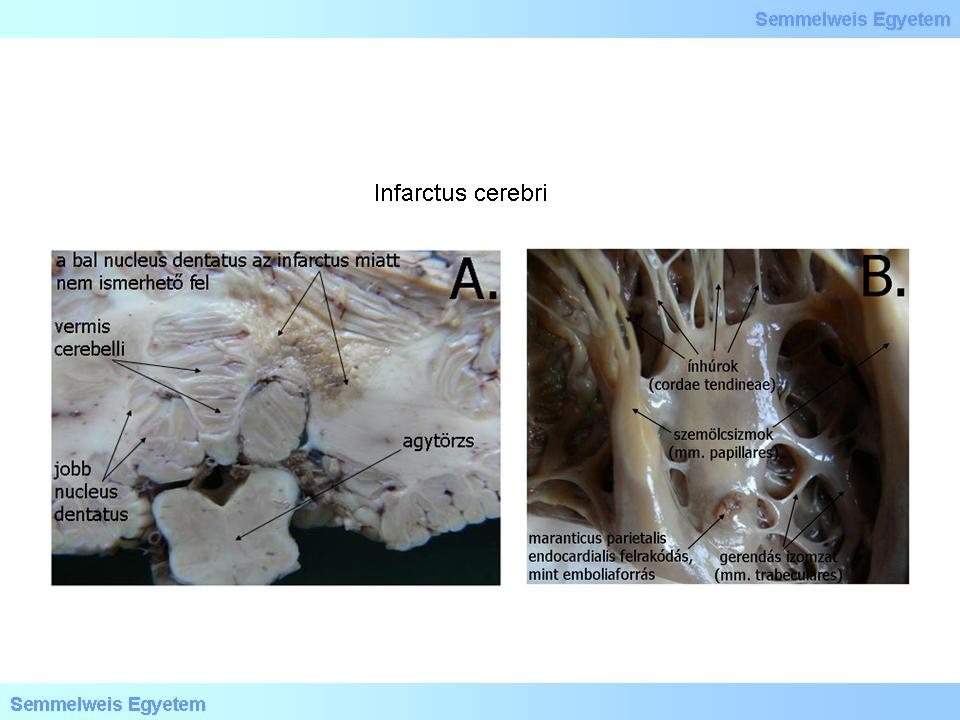
Macrographs 5A-B: A: Subacute infarction before cavitation, destroying the area of the left nucleus dentatus, on the horizontal cut-surface of the brain stem and the cerebellum. B: The source of the emboly causing the infarction was a marantic endocarditis. (A favor of Péter Molnár; University of Debrecen, Medical and Health Sciences Center, Department of Pathology)
|
Based on their appearance infarctions are divided into two groups: anaemic, or white, and haemorrhagic, or red (cerebral softening, emollitio cerebri), and both of them are caused by vascular occlusion. Haemorrhagic infarction usually develops as a secondary haemorrhage in the affected, softened area (macrograph 6). Generally, the solution of the primary occlusion is in the background. The circulation on the necrotic area can restart (so called reperfusion) by endogen thrombolytic (enzyme) processes, or by iatrogenic (associated with medical intervention) reason, due to anticoagulant therapy.
|

Look into the pictures!
|
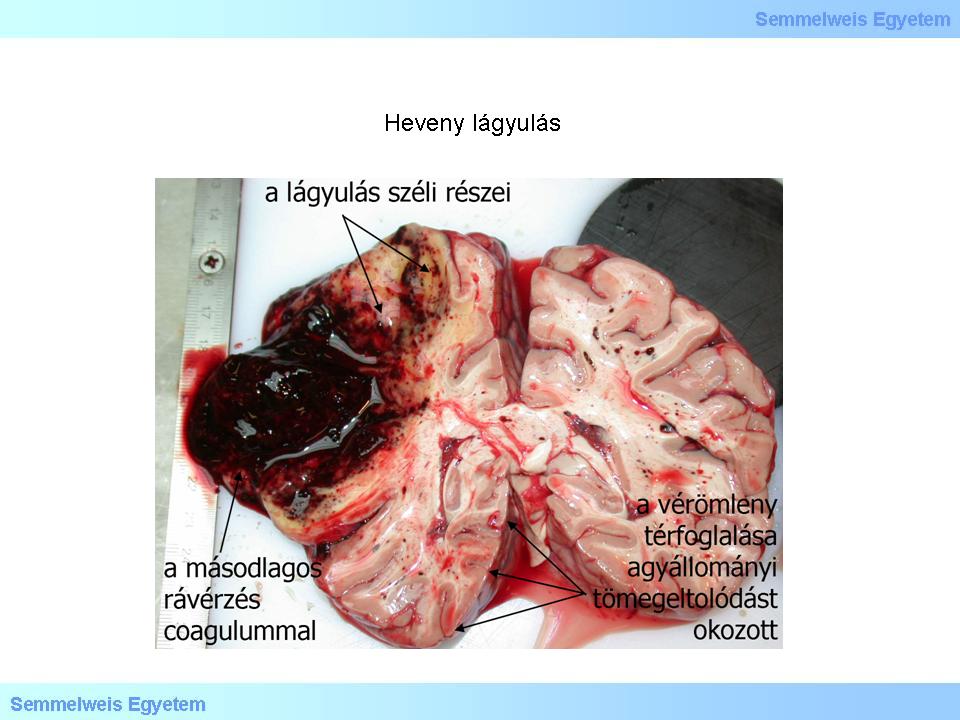
Macrograph 6: The original, acute necrosis of the brain tissue, due to softening, can only be observed circumstantially at the marginal parts of the affected area, because of the secondary haematoma. The significant increase of the volumen affects also the volume-distribution of the brain. (From the image-archive of the Semmelweis University, 2nd Department of Pathology–collection of Attila Kovács)
|
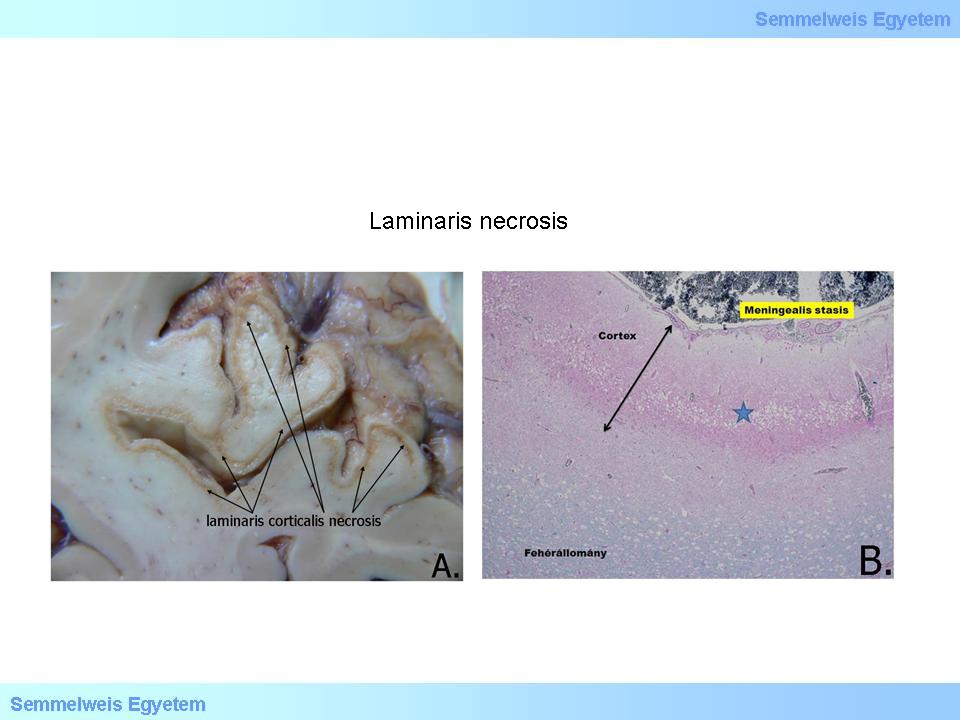
Macrographs 7A-B: A: At the bottom left corner of the picture, a relatively intact, well distinctive grey- and white matter can be observed, while in the middle, at the cortical region a track-like light dun pigmentation shows, that is laminar necrosis. B: Histological picture of laminar necrosis (HE; 150x). (A favor of Péter Molnár; University of Debrecen, Medical and Health Sciences Center, Department of Pathology
|

Macrographs 8A-C: A-B: Macroscopic picture of the so called ”watershed” infarction. C: In the area of chronic necrosis, with MRI, hyperdensity is detected. (A favor of Péter Molnár; University of Debrecen, Medical and Health Sciences Center, Department of Pathology)
|

Macrographs 9A-D: The so called „respirator brain”. A-B: The dirty, dun cortical pigmentation is the result of in vivo autolysis. C-D: Destruction of the cerebellar cortex, due to in vivo putrefaction, can be observed. (A favor of Péter Molnár; University of Debrecen, Medical and Health Sciences Center, Department of Pathology)
|
Chronic lesions evolve from those mentioned above: definitive infarctions can be seen in borderline zones, yellowish – because of the phagocited and metabolized fat-like material -, and russet – because of the hemosiderine that comes from the microscopic bleeding -, impressed areas are left behind, where cyst do not form eventually. A chronic, macroscopically well observable residuum of larger necroses is a cavity (in fact, a pseudo-cyst), in the site of colliquated tissue. (Macrograph 4).
A special form of the chronic nodular lesions with tissue loss is the so called lacunar infarction.
|

Look into the picture carefully!
|
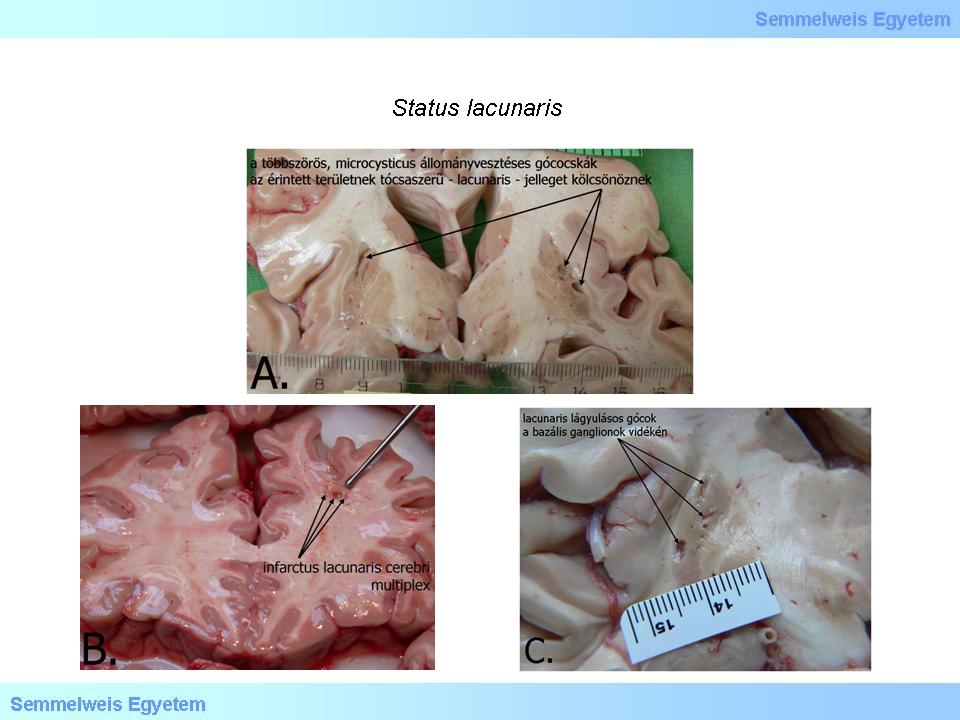
Macrograph 10A-C: Close picture of status lacunaris. On the larger branches of arteries, pathognomic (lipo)hyalinosis. (A, C: A favor of Péter Molnár; University of Debrecen, Medical and Health Sciences Center, Department of Pathology; B: From the image-archive of the Semmelweis University, 2nd Department of Pathology–collection of Attila Kovács)
|
Histologically, acute lesions can be characterized by various levels of neuronal ischemia: intensive cytoplasmic eosinophilia, shrinking, and then dissolving of the nuclei (karyopyknosis, and karyolysis). Neuropil is unchanged at the beginning, but over time, (micro)vacuolisation develops, to different extents.
Typical lesion is the laminar necrosis: track-like loss of cells in the neocortex. In more severe cases, the complete cell- and tissue necrosis is not limited in the lamina III and V, but the whole cortex necrotises.
Clinically, the consequences of the ischemia are determined by the localization of the occlusion, and the available capacity of anastomoses. Intact circle of Willis can even provide circulation in case of the occlusion of either one of the major arteries, however, the posterior part is less defended. The overlaps across the perfusion zones of the big branches of the arterial circle may function as a compensatory reserve. This is the reason why the extension of infarctions are usually smaller compared to the perfusion area of the occluded artery.
|
|