|
IV./2.3.: Puerperal uterus – puerperal fever
IV./2.3.1.: Healthy puerperium (physiological puerperium)
|
 |
The period directly after childbirth (post partum) is called puerperium). Puerperium is divided into two parts: early puerperium is the first 10 days after childbirth (postpartum); while late puerperium lasts from day 10 until the 5-6th week. Under physiological circumstances the size of the puerperal uterus (postpartum uterus) is equivalent to its size on the 20th gestational week, with a 3-centimetre-thick wall on average, and a fundus below the umbilicus with 2-4 fingerbreaths. The uterine cervix is dilated, floppy, while the corpus is highly contracted. After childbirth (although reducing constantly) the uterus still exceeds its regular size. Its postpartum involution occurs gradually, in around 6 weeks.
This phenomenon has a hormonal reason, since the placental hormones, which have maintained the rich blood supply and increased cellular metabolism of the womb deplete within days . Oxytocin, a hormone of the pituitary gland helps the permanent contraction of the uterus (these are the so-called postpartum tormina ), the degradation of smooth muscle cells, the narrowing of the vascular lumina, the degeneration of spiral arteries and the involution of the organ. The uterus weighs around 1000 grams after childbirth, and is 15 cm by its longitudinal axis. Within a week, it becomes 500 g heavy and 12 cm long, within 2 weeks 250 g and 10 cm, while after 6 weeks only 50 g and 7 cm. The first ovulation occurs earliest on the 6th week after the birth.
After childbirth until the relatively fast (ranging from a few days to a week) regeneration of the mucosa the internal surface of the womb is one confluent wound area covered with blood clots. During this period the uterus is an entry gate with an extensive surface for pathogens. The infections are usually prevented successfully by the fast contraction and regeneration of the surface, and by the developing inflammatory barrier (a protective layer impregnated with enzymes, consisting of white blood cells and fibrin). After a week the epithelialization begins from the deeper layers. The process is the slowest at the location of the placental adherence.
|
 |
Regeneration occurs without scarring. From the uterus a secretion of diverse quantity (more in the beginning, less later) called lochia is discharged. Lochia is a wound fluid, which contains necrotic decidua portions, liquefied blood clots and leukocytes. Although bacteria are present in the uterine corpus already after 6-12 hours after giving birth, these are emptied with the bactericide discharge. Six-ten days after childbirth the mucous plug of the cervix is restored and the uterine space becomes sterile. The cervix regains its regular shape within 8-10 days. The tone of the vagina is regained very fast as well due to the good blood supply, the full venous braids and the contraction of smooth muscle cells.
IV./2.3.2.: Pathological childbed (pathological puerperium)
|
 |
Postpartum pathological phenomena are complex, diverse disorders (i) bleeding abnormalities ; (ii) childbed infections (childbed fever – puerperal fever or sepsis); (iii) thrombosis, thrombophlebitis; (iv); puerperal mastitis; (v) postpartum/puerperal psychosis; (vi) bone and joint problems.
IV./2.3.2.1.: Abnormal bleeding
Impaired involution (subinvolution) of the uterus is one of the reasons behind abnormal uterine bleeding. The condition is present after the overdistension of the uterus (polyhydramnion, twin pregnancy, oversized foetus) (1st micropicture), or after tumours of the uterine wall (usually intramural leiomyoma), or after inflammations of the mucous membrane. It is very common in case of lacking nursing, because of an insufficient oxytocin effect. It is accompanied by a small quantity of prolonged bleeding and stagnating lochia. Puerperal endometritis can also cause abnormal bleeding. Due to its importance the condition is discussed in its own chapter. A retained placenta (placental or cotyledonal retention) can lead to severe, life-threatening complications. The condition is characterized by a rich, fresh bleeding during the first or second postpartum week.
|

Study the picture!
|
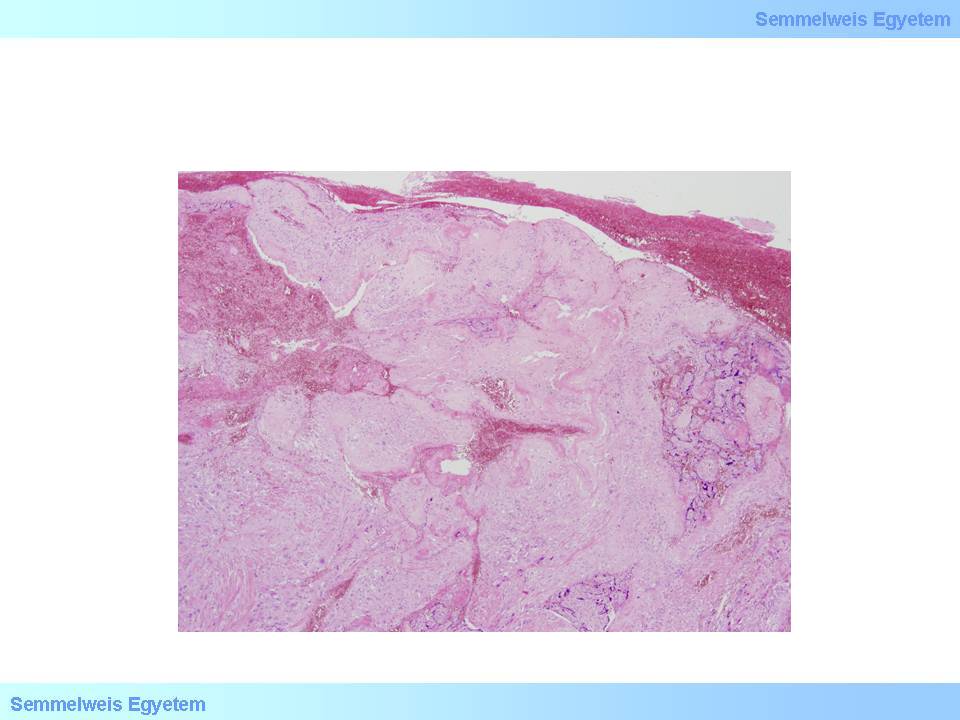
1st microphoto: Subinvolution. The material derives from hysterectomy, which was performed because of an atonia after gemini pregnancy. The uterine cavity is covered with focally haemorrhagic, inflamed uterine residua, the myometrium is intruded by decidual parts. (HE; 100x) (From the photo archive of the Semmelweis University 2nd Institute of Pathology – collected by Ildikó Szirtes).
|
If coagulum deposits onto the retained placenta, it forms a polypous structure (placental polyp). The retained, diminishing tissue forms an excellent culture for ascending bacteria: untreatedly (curettage) the retention is soon accompanied by infections (endo-myometritis) and generalized infections (sepsis).
Thrombus rejection occurs on the 2-3rd week of uncomplicated childbed in the form of rich bleeding: a thrombus occluding a bigger uterine vessel is rejected.
An incomplete regeneration of the endometrium can originate from the disturbed epithelization of the placental attachment. It can be caused by a submucous leiomyoma developing at that location, by a scar line deriving from a previous Caesarean section; as a symptom, spotting can occur.
Abnormal bleedings resulting from malignant tumours are luckily rare, but the possibility has to be considered, especially if the expectant mother belongs to a population at risk. According to the traditional point of view the relative immune tolerance during pregnancy favours tumour development, so changes of precancerous state can progress rapidly, and progressive malignant conditions can develop during the nine months of the pregnancy.
|
 |
Recently this proposition has been questioned by a few studies. According to their observations oncological outcome during the pregnancy is similar to the outcome of the control population. They also remark that foetal development would not even be affected by neoadjuvant chemotherapy. These results indicate that pregnancy is such a complex life situation, where an increased medical care is needed (especially until a professional consensus regarding gestational tumour progression is developed, since both negligence and excessive interventions can harm maternal and also foetal lives.
In this age and patient group cervical cancer and preceding dysplasias have to be considered. In case of women who attend cancer screening regularly these factors are known to the medical staff and whether to keep or terminate the pregnancy can be decided based on these information, also considering other circumstances of life. An especially careful consideration is needed if the HPV demonstrable from the lesion belongs to a high-risk group. During an unassistanced pregnancy of women who did not attend cancer screening previously, the development of a malignant tumour can be a real surprise. Choriocarcinomas are more frequent in case of women with previous mola pregnancies. It follows the end of the pregnancy relatively late, in the form of bleedings. Endometrial carcinomas are expressly rare in this age group.
IV./2.3.2.2.: Puerperal infections
|
 |
The history of medicine has recorded massive puerperal epidemics in the hospitals of the 17th-19th century, during which 10-15% of mothers died in the crowded institutions, which were not following even the most basic rules of hygiene. With Semmelweis and his seminal regulations this rate dropped to under 1% in places led by his disciplines. Nowadays postpartum infections occur in 2-5% of cases, with a mortality rate of 2-5‰. Pathogens enter the body usually directly (by manual examinations, treatment devices, bedding, and nursing stuff). They settle around injuries, erosions, effusions. Impoverishment of the body (exhausting delivery, significant blood loss) usually favours infections.
The majority of pathogens include:
-
- Staphylococcus,
-
- Streptococcus ,
-
- Enterococcus,
-
- E. coli ,
-
- Pneumococcus,
-
- Pseudomonas aeruginosa,
-
- or a combined flora consisting of a mix of the above mentioned pathogens
Forms of infection by their extension:
|
 |
-
1. puerperal ulcer;
-
2. endo-myometritis;
-
3. adnexitis;
-
4. parametritis;
-
5. pelvic peritonitis/peritonitis;
-
6. sepsis.
In case of postpartum ulcers pathogens can enter the body through injuries, ulcers on the vaginal, pubic and perineal area. The wound is covered with purulent plaques, which are circumscribed for some time, but can lead to sepsis as well.
In endo-myometritis the inflammation spreads onto the mucosa and to the muscular wall of the uterus, causing the appearance of putrid lochia, spontaneous pain and pain occurring upon press. The condition is accompanied by a bad general condition and high fever. Histologically an acute inflammation of the uterine mucous membrane is present if in the non-haemorrhagic, focally necrotic endometrium a great number of leukocytes are present. Neurophil cells compose microabscesses in the stroma, and infiltrate the glandular chambers as well (2nd microphoto). The condition usually develops in the second week of the postpartum period. If negligent care delivers pathogens close to the intrauterine wound (like in Semmelweis’ era) or something (e.g. retention of the placenta or the decidua [placental or decidual retention]) prevents the regeneration and retraction of the uterine surface, then the surface can be infected by a mass of pathogens.
|

Study the picture!
|
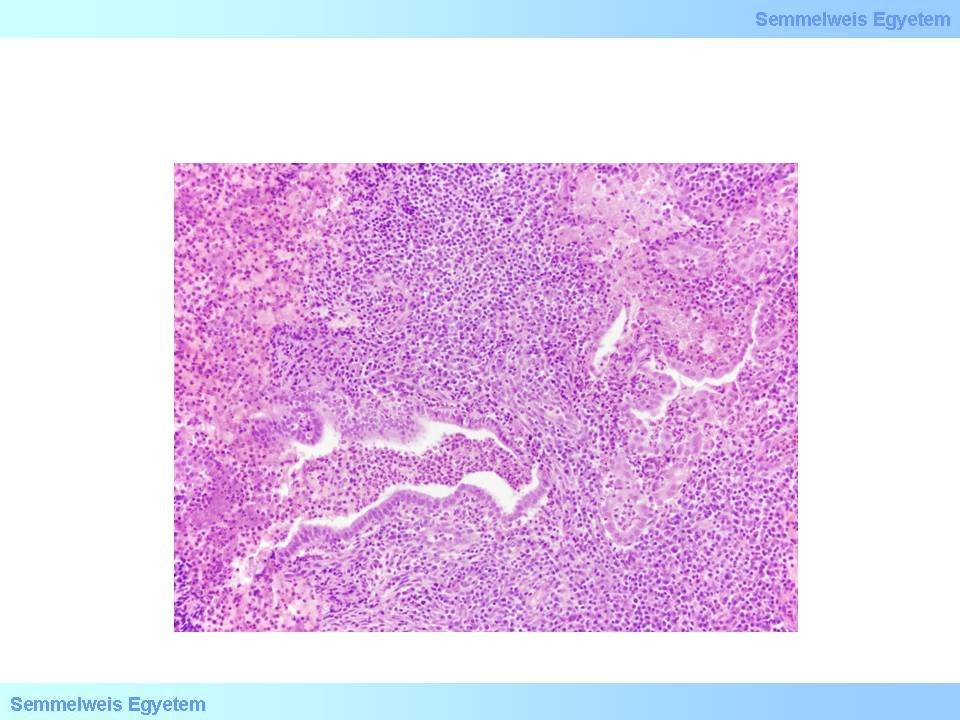
2nd microphoto: Acute endometritis. Endometrial stroma or endometrial glands are filled with neutrophil granulocytes (HE; 400x) (From the photo archive of the Semmelweis University 2nd Institute of Pathology – collected by Ildikó Szirtes).
|
The internal surface of the uterine cavity is covered with a thick, fibrinous-purulent exudate containing placental residua or in case of retention by tissue debris. The applied uterine manipulation can lead to an endotoxin shock and to the explosive spread of the infection. The pathogen is often the S. pyogenes (a Gram-positive bacterium, which belongs to the ß haemolitic A group of Streptococci), which is responsible for the inflammatory reaction, causing a special from of wound infections, the postpartum fever (puerperal endometritis, childbed endometritis). If the ascending infection spreads canalicularly through the fallopian tubes, an adnexitis develops. High fever, an area sensitive to pressing, acute pain, malaise endure or worsen. If pus occurs in the tubes, a pyosalpinx develops. With the inflammation of the ovaries oophoritis, with the infiltration of the surrounding tissues a tuboovarian abscess develops (1st macrophoto, 3rd microphoto).
|

Look at the pictures and analyze them!
|

1st illustration: Uterus puerperalis (Kiss Balázs gyűjtése): (1) Corpus uteri; (2) Cervix uteri; (3) Vagina; (4) Ligamentum latum uteri; (5) Tuba uterina; (6) Ligamentum ovarium proprium; (7) Endometritis puerperalis
|
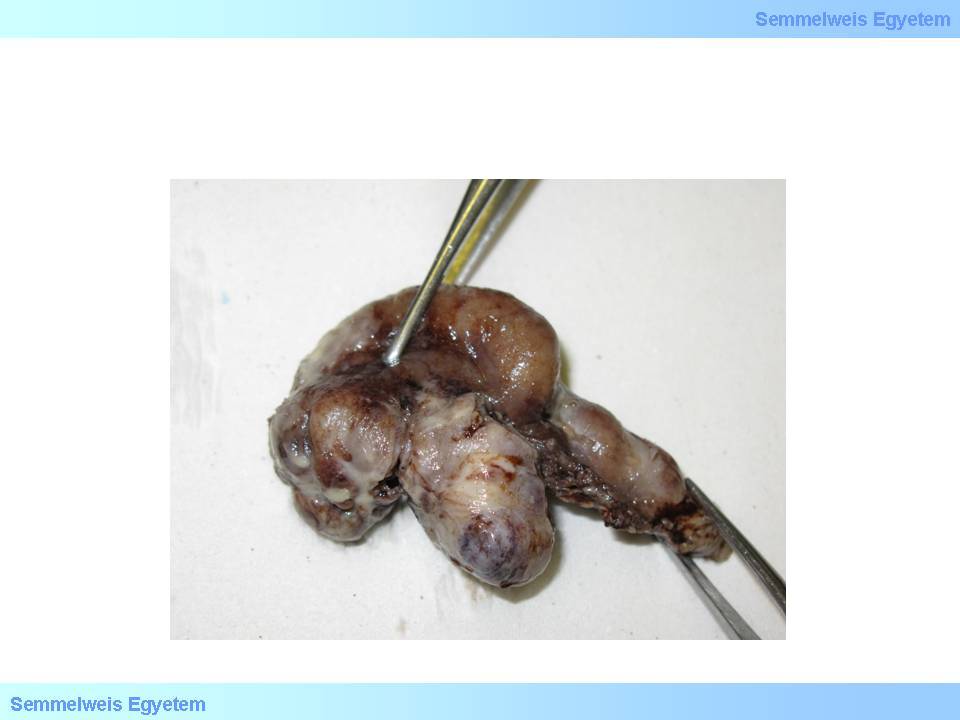
1st macrophoto: Tuboovarian abscess. The inflammation of the uterine adnexes forms a pelvic conglomerate. The surface is covered by a purulent exudate. (From the photo archive of the Semmelweis University 2nd Institute of Pathology – collected by Attila Kovács and Ildikó Szirtes).
|
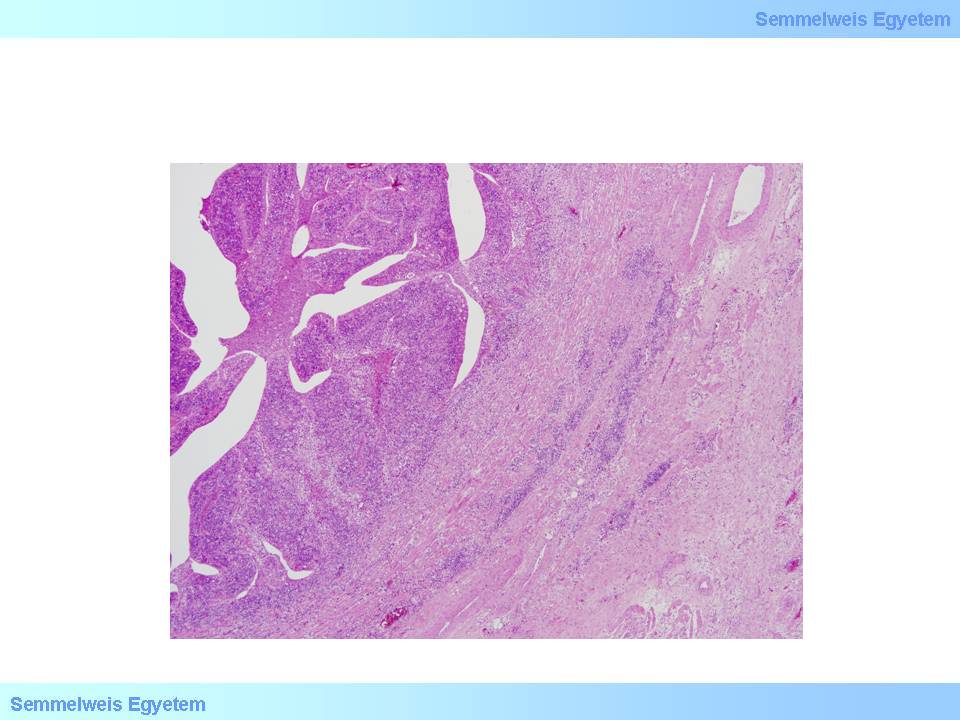
3rd microphoto: Tuboovarian abscess. In the neighbourhood of the fallopian tube, which was distorted by the infiltration of mixed inflammatory cells fibrosis, which also includes the ovaries (not present on the picture) can be observed. The connective tissue is also infiltrated with inflammatory cells. (HE; 200x) (From the photo archive of the Semmelweis University 2nd Institute of Pathology – collected by Ildikó Szirtes).
|
If a lymphogenic spread of the inflammation is present, parametritis, a parametrial abscess develop. All forms of the inflammation of the tissue, which surround the uterine corpus (adnexitis, parametritis, oophoritis, tuboovarian abscess) lead to an increased tenderness to palpation. The inflamed mass results in an ’inflammatory conglomerate tumour’. Spreading through the fallopian tube almost always results in the propagation of bacterial inflammation onto the surrounding peritoneum; a pelvic peritonitis develops. The same condition occurs if an abscess surrounding the uterus ruptures into the abdomen. Pelvic inflammations spreading retrogradely, through veins can be complicated by the thrombosis of the femoral veins, which causes a severe disorder with lower leg pain and swelling (phlegmasia alba dolens).
|

Look at the pictures and analyze them!
|

2st illustration: Uterus puerperalis (Kiss Balázs gyűjtése): (1) Corpus uteri; (2) Cervix uteri; (3) Vagina; (4) Ligamentum latum uteri; (5) Tuba uterina; (6) Ligamentum ovarium proprium; (7) Ovarium; (8) Ligamentum cardinale uteri; (9) Ureter; (10) Parametritis, parametrialis abscessus ; (11)Tubo-ovarialis abscessus
|
If peritoneal adhesions isolate the process to the pelvis, a so-called Douglas abscess develops. When an isolation like this is lacking, a life-threatening diffuse, purulent peritonitis, an acute abdomen, a paralytic ileus develop . Puerperal sepsis, the most severe puerperal infection can develop from any of the above listed infection types. It can develop in a hyperacute, acute form, but a prolonged, chronic sepsis can occur as well. The previous types result in death within a few days, the latter leads to the development of multiplex abscesses in multiple organs, including the lung, the heart valves, the heart muscle, the kidney and the liver.
|
 |
The clinical picture is dominated by the developing shock: a severe, bad general condition, frequent breathing (even 40/min), filiform, depressible pulse (120-140/min), shudders, shivers, and shortness of breath, restlessness or sometimes the opposite: delirous-euphoric state, septic-undulating or the opposite: a continuous fever, and oliguria. With the development of a so-called multi-organ failure – MOF icterus occurs as well. If finally DIC (disseminated intravascular coagulopathy)develops, then haemophilia and smaller-bigger bleedings occur all over the body.
It should be mentioned that Ignác Fülöp Semmelweis has developed the antisepsis principles (1847) during the observation of puerperal fever in a period when pathogens causing disorders have not been discovered yet. These guidelines are nowadays considered as important milestones of medicine.
|
|