|
II./1.1.: Large intestine (intestinum crassum)
II./1.1.1.: General characteristics
|
 |
The large intestine forms a 'frame’ around the loops of the small intestine, which are found in considerable irregularity in the abdominal cavity. The large intestine is responsible for the absorption of salt (sodium) and water, it has no digestive function.
Its length is about 150 cm. Parts: the small intestine ends at the ileocecal junction and this is the beginning of the colon: its first part, the cecum is found in the right iliac fossa. The cecum is followed by the ascending, the transverse, the descending and the sigmoid colon; then, in the pelvis the rectum is situated which finally ends with the anus.
The transverse colon exhibits on its both sides well defined flexures (left and right colic flexures) which demarcate the transverse colon from the ascending and descending colon. To identify whether a piece of small or large intestine is placed in front of us, is not an easy task, especially during surgery. In contrast with the traditional names of the bowel (i.e. „small” and „large” intestine) we cannot surely decide it according to the diameter of the intestine. Since the surgeon must be clearly informed about the structures of the abdominal cavity, it is necessary to know the three macroscopic features of large intestine which help us to clearly separate the small intestine from the colon with the naked eye, even during surgery (Fig. 1.):
|

Study the drawing / figure!
|

Figure 1.: The gross anatomical features of the colon(Kiss Balázs)
(1) Haustra coli, (2) Tenia omentalis, (3) Tenia mesocolica, (4) Tenia libera, (5) Appendices epiploicae, (6) Omentum majus, (6) Colon keresztmetszet
|
II./1.1.1.1.: Haustra coli
are the characteristic spherical sacculations (pouches) of the colon (areas between the semilunar folds which are seen inside the colon). Although these bulges appear always according to the actual smooth muscle contractions, they still provide a safe basis to identify the large intestine - either during radiography or surgery.
II./1.1.1.2.: Teniae coli
|
 |
the wall of the colon - in contrast with the small intestine - has no complete outer longitudinal muscle layer along the total circumference of its wall. The outer longitudinal muscle layer is rather reduced to longitudinal ribbons easily seen with the naked eye (tenia = ribbon, band). The 3 typical teniae can be identified on the transverse colon: the mesocolic, omental and free teniae (tenia mesocolica, tenia omentalis and tenia libera). These muscle bands are continuous with the teniae of the ascending and descending colon, although in a twisted course. At the lower end of the cecum the 3 teniae meet, clearly 'pointing' to the appendix, which is easy to find this way, by following the teniae. However, there is no tenia (since the outer muscle layer is complete) on the appendix and rectum; only 2 teniae can be found on the sigmoid colon.
II./1.1.1.3.: Appendices epiploicae
Appendices epiploicae (epiploic appendices): small peritoneal-lined pendulous protuberances (appendages) of the colon, filled with fatty connective tissue (histologically comprised of the tunica serosa and the tela subserosa). Since they might contain end arteries supplying the colonic wall, their surgical removal should be avoided.
The parts of the large intestine:
|
 |
-
- coecum;
-
- appendix (vermiform process);
-
- ascending colon;
-
- right colic flexure (or hepatic flexure);
-
- transverse colon;
-
- left colic flexure (or splenic flexure);
-
- descending colon;
-
- sigmoid colon;
-
- rectum;
-
- anus.
II./1.1.2.: Coecum
A downwards directed, blind pouch (Caecus [Latin] = blind) of the colon, located at its beginning. The ileum opens with the ileocecal orifice (ileocecal ostium) into the cecum, approx. 4-5 cm above the lowest point of the cecum (Fig. 2.). The orifice exhibits the ileocecal valve (Bauhin’s valve), which controls the unidirectional flow of the intestinal content into the cecum - although this orifice cannot be considered as a hermetically sealed opening. On the outer surface of the cecum the three teniae are recognizable, which, leading downwards, ’point’ to the appendix, making it easy to find. Its peritoneal relations vary - sometimes a shorter or longer peritoneal duplicate is found, in other cases the cecum is tightly attached to the posterior abdominal wall. At the ileocecal junction, above and below the ileum peritoneal pouches can be formed (sup. and inf. ileocecal recesses), into which loops of small intestine can get stuck (potential internal hernia can develop here).
|

Study the drawing / figure!
|
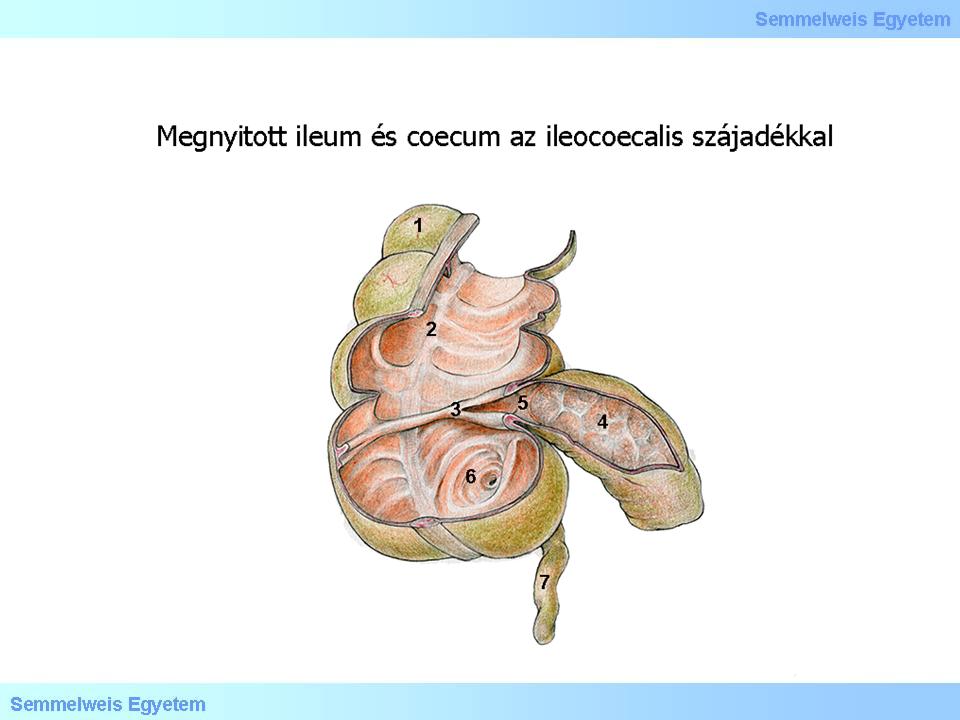
Figure 2.: Ileum and cecum, opened; the ileocecal orifice can also be seen. The ileocecal valve (of Bauhin) and the orifice of the appendix are clearly visible (Kiss Balázs).
(1) Haustra coli, (2) Tenia coli, (3) Valva ileocoecalis, (4) Ileum, (5) Ostium ileocoecale, (6) Ostium appendicis vermiformis, (7) Appendix vermiformi
|
II./1.1.3.: Appendix (vermiform appendix, vermiform process)
|
 |
The vermiform process (vermis= worm) or appendix is a part of the colon having major clinical significance; it gets surgical importance due to its life-threatening inflammation (acute appendicitis). Located in the lower right abdominal area, where different diseases of other organs (most often the ureter, the ovary, the uterine tube, the urinary bladder) can cause severe pain also, resulting differential diagnostic difficulties (see the differential diagnosis of "acute abdomen").
Basically, the appendix is a lymphoid organ "guarding" at the junction of the small and large intestines, serving as immunological „border-control” between the bacterium-rich large intestine and the small intestine which is normally poorly colonized with bacteria. In the absence of appendix (in case of its surgical removal), however, no significant immunological deficit can be expected. On average, 6-10 cm long (but can vary between 2 and 25 cm), 6-8 mm thick, blind-ending evagination of the colon (its blind end causes certain risks: the bowel content can get stuck here causing the obstruction of the lumen and subsequent inflammation). Usually starts 2,5 cm below the ileocecal junction. Its orifice often exposes a small valve (Gerlach’s valve). The three teniae seen on the outer surface of the cecum help us to find the appendix: the teniae, as followed downwards, end up at the appendix and form its complete outer longitudinal muscle layer.
Peritoneal relations: the appendix is a totally intraperitoneal organ; its own small peritoneal duplicate is the mesoappendix (formerly known as mesenteriolum processus vermiformis). The blood vessels and nerves course to the appendix in the mesoappendix. Position: due to its mobility allowed by the mesoappendix, there are numerous positional variations: it can hang down into the pelvic cavity (pelvic position); quite often seen in retrocecal position or turning to the left, or also passing upwardly; can be located in front or behind the terminal loop of ileum.
Due to developmental anomalies (situs inversus, malrotation) the appendix can be found at other sites of the abdominal cavity as well: in the left iliac fossa ( instead of the right one), if the umbilical loop rotates only 90° instead of 270° - in this case the whole colon is located in the left side, in the lower part of the abdomen. The vermiform process can also be found under the liver (subhepatic cecum and appendix) - if the umbilical loop rotates only 180° and the cecum does not descend. In these cases the atypical symptoms can cause more headache and diagnostic difficulties to the physician examining the patient. The abdominal wall projection of the typically located appendix is the McBurney’s point (at the lateral one-third of the distance from the right anterior superior iliac spine to the umbilicus): the tenderness or pain of this point is pathognomonic for the diagnosis of appendicitis.
|
 |
Blood supply: the ileocecal artery (ileocolic a.), a branch of the superior mesenteric artery gives the appendicular artery, reaching the appendix inside the mesoappendix. The tip of the appendix is the weak point of the arterial supply since this area is nourished by (practically) end arteries. In case of inflammation the wall of the appendix is edematously thickened; it can lead to the compression of the smaller vessels, resulting thrombosis in them. In this case, the wall of the appendix necrotizes, causing a very severe complication: perforation may occur, with all of its consequences: first localized, later diffuse inflammation of the peritoneum (peritonitis); the mortality of diffuse peritonitis is high, even nowadays. Therefore it is important to know the symptoms and make the early diagnosis of appendicitis, followed by the correct surgical treatment in time. Lymphatic drainage: via the 1-2 lymph nodes situated in the mesoappendix into the superior mesenteric lymph nodes. Innervation: the appendix receives parasympathetic fibers from the vagus nerve and sympathetic nerves from the superior mesenteric plexus. The typical pain felt by the inflammation is mediated by sensory nerves of the Th10 segment.
II./1.1.4.: Ascending colon
The ascending colon is the upward continuation of the cecum, but cannot be separated by a sharp border; approx. 20 cm long part of the colon. Courses upwards at the right side of the abdominal cavity; then, reaching the right lobe of the liver makes a turn (right colic flexure or hepatic flexure), after that is continued into the transverse colon. Peritoneal relations: since the posterior surface of the ascending colon is fused with the posterior abdominal wall, the peritoneum covers only the two sides and the anterior surface of the ascending colon (semi-intraperitoneal position). On its right side a groove formed by the peritoneum (the right paracolic gutter or right paracolic sulcus/ right paracolic space) allows passage for any fluid (eg. inflammatory effusion) from the upper part of the abdomen downward.
II./1.1.5.: Right colic flexure (hepatic flexure)
Found at the right lobe of the liver, its angle is slightly smaller than 90°; it is the border between the ascending and transverse colon.
II./1.1.6.: Transverse colon
|
 |
Topography: when the abdomen is opened, at first is hidden, since the fatty peritoneal layers of the greater omentum (hanging down from the greater curvature of the stomach like an apron) cover it. Just after lifting the greater omentum can be revealed the position of the transverse colon, which is -somewhat contrary to its name- found at a rather curved-line hanging down. Its length is approx. 45 cm. Peritoneal relations: a typical intraperitoneal intestine, having a long peritoneal duplicate (transverse mesocolon) originating from the posterior abdominal wall. Therefore this is the most mobile part of the large intestine, usually hangs deep down in the abdomen, above the loops of small intestine.
The transverse mesocolon contains its blood vessels (branches of middle colic artery and vein). The attachment line of the transverse mesocolon on the abdominal wall crosses anteriorly the (retroperitoneally located) descending part of duodenum and head of pancreas; then courses in front of the duodenojejunal flexure, crosses the capsule of the left kidney, ending at the left colic flexure.
The upper surface of the transverse colon is fused with the greater omentum which hangs down from the stomach. As mentioned above, the names of the teniae were given according to their location at the transverse colon:
-the mesocolic tenia is found at the attachment of the transverse mesocolon;
-the omental tenia is fused with the greater omentum;
-and finally, freely seen (in between) the third muscle ribbon, the tenia libera.
The four layers of the greater omentum fuse not only with the transverse colon, but also with the double peritoneal layers of the transverse mesocolon, therefore the gastrocolic ligament (found between the transverse colon and the stomach) is originally formed by the fusion of six peritoneal layers.
II./1.1.7.: Left colic flexure (splenic flexure)
|
 |
This flexure is found in the left hypochondrium, at approx. 3 transverse finger width higher than the hepatic flexure; exposing a sharper bend than the hepatic flexure. This flexure indicates the left end of the transverse colon. Here one can find a peritoneal band, the phrenicocolic ligament, which anchors this part of the colon to the diaphragm but is also important in supporting the spleen (sustentaculum lienis).
II./1.1.8.: Descending colon
Topography: the descending colon is located on the left side of the abdomen, passing from the left colic flexure into the left iliac fossa. Fused with the posterior abdominal wall, coursing down in front of the lateral edge of the left kidney. Post-mortem is usually only a finger-breadth thick. In living humans it is the narrowest part of the large intestine (explaining the obstructive symptoms occurring here most often). The length of it is 22-30 cm. Peritoneal relations: its posterior surface - similarly to the ascending colon – is fused with the posterior abdominal wall which is located immediately behind it, therefore the peritoneum covers only the two sides and the anterior part of it (semi-intraperitoneal location). On its left side, between the abdominal wall and the descending colon a peritoneum-lined depression is found (left paracolic gutter, left paracolic space), where any fluid can move down from the splenic flexure area (the area below the phrenicocolic ligament) to the pelvis.
II./1.1.9.: Sigmoid colon
|
 |
Topography: having an S-shaped curvature, the sigmoid colon courses from the left iliac fossa to the pelvis; approx. 40 cm long. On its outer surface the appendices epiploicae are particularly long, its teniae are fused to form a broader anterior and a posterior muscle bands. Peritoneal relations: completely intraperitoneal; because having a long peritoneal duplicate (sigmoid mesocolon, mesosigmoid) is rather mobile, so its position is quite various. In the mesosigmoid one can find the vessels (sigmoid arteries and veins supplying the sigmoid colon. The easiest way to identify the beginning and the end of the sigmoid colon is to visit the duplicate of mesosigmoid, since the descending colon and the rectum have no peritoneal duplicates. The mesosigmoid exhibits peritoneal depressions called recesses, into which small intestinal loops may become entrapped, causing internal hernias.
II./1.1.10.: Rectum
Contrary to its name (rectum = straight) the rectum is a curved intestine: at its beginning, at the sigmoid colon-rectum border one can find the flexura rectoromana, then two flexures are seen in the sagittal plane: the sacral flexure (situated in the concavity of the sacrum, anteriorly concave bend and the perineal flexure (found at the perineum, backward curved bend, turning around the coccyx). Therefore the final opening, the anus looks backwards (thus reducing perineal and genital faecal contamination). These conditions are important during endoscopic examinations (rectoscopy and colonoscopy).
The initial part of the rectum is the expandable ampulla recti, while the portion above the anus, the anal canal is closed except during defecation.
|
 |
Peritoneal relations: the rectum, being 12-15 cm long, only its upper one-third is partly (from anterior and lateral) surrounded by peritoneum (semi-intraperitoneal), but downwards gradually loses its peritoneal covering: the middle third is found behind the peritoneal cavity (retroperitoneal), the lower part is below it (infraperitoneal). The peritoneum proceeds from the rectum anteriorly:
-
- in men it covers the urinary bladder,
-
- in women moves to the posterior fornix of vagina and uterus.
This way peritoneum-lined depressions are formed: the rectovesical pouch in men and the rectouterine pouch (of Douglas) in women - these are the deepest points of the abdominal cavity in a standing human. Abnormal fluids of any origin (eg. inflammatory exudates, blood) are collected here from the peritoneal cavity – giving the clinical significance of these pouches.
The anterior wall of the rectum is in contact with the prostate and seminal vesicles in men, this topographic relationship makes the rectal digital examination (examination of the prostate with the physician’s finger through the rectum) possible. The relationship with the important levator ani muscle (pelvic diaphragm at the floor of lesser pelvis) has also basic significance. The voluntary innervated striated muscle sphincter, the external anal sphincter muscle is closely connected with it. The internal anal sphincter muscle of the rectum is a pronounced thickening of the internal circular smooth muscle layer, having no voluntary innervation.
II./1.1.11.: The arterial blood supply of the large intestine
The midgut-derived intestines receive their blood supply from the branches of the superior mesenteric artery, therefore the proximal part of the colon, from its beginning to the left colic flexure gets its arterial blood from here. The parts of the colon situated distally from the left colic flexure are derivatives of the hindgut, that’s why supplied by the inferior mesenteric artery. The very last part (the lower third of the rectum) belongs to the supply area of the internal iliac artery.
II./1.1.11.1.: Superior mesenteric artery
|
 |
The ileocolic artery is a branch of the superior mesenteric artery (to the cecum); the ileocecal artery gives the appendicular artery below the ileum. The right colic artery runs to the ascending colon, the middle colic artery supplies the transverse colon. Before these colic arteries reach the intestine they form loops or arcades (marginal arcades), the branches of these arcades, being functional end arteries feed the different parts of the colon. At some places (eg. in the mesosigmoid) secondary or tertiary arcades may also develop. The blood vessels pierce the smooth muscle layer of the colon; the sites of piercing are weaker points of the colonic wall (potential diverticulum formation). The blood supply is usually the richest in the tela submucosa (arterial plexus).
II./1.1.11.2.: Inferior mesenteric artery
The inferior mesenteric artery gives the left colic artery to the descending colon, the sigmoid arteries course in the mesosigmoid to the sigmoid colon, whereas the superior rectal artery is responsible for the blood supply of the upper third of the rectum. These arteries also create arcade-like anastomoses. We have to mention the anastomosis created between the two arterial systems (the superior and inferior mesenteric arteries): at the left colic flexure the (greater) Riolan’s arch is created by the middle colic and the left colic arteries. However, this anastomosis still provides a relatively poor blood supply to the splenic flexure area, that’s why in this region problems with the vascular supply (ischemic diseases) might more often occur. There is an anastomosis between the superior rectal artery and the last sigmoid artery (a. sigmoidea ima). The site where this anastomosis meets the superior rectal artery is called the Sudeck’s point. The Sudeck’s point has - perhaps a little overestimated - surgical significance: when doing rectal surgery, the superior rectal artery can only be ligated proximally from this point in order to maintain the normal arterial blood supply of the rectum. The blood supply of the lower two-thirds of the rectum: the paired middle rectal arteries (direct branches of the internal iliac artery) and the also paired inferior rectal arteries (branches of the internal pudendal artery).
II./1.1.12.: The venous drainage of the large intestine
|
 |
The veins of the colon, including also the upper third of the rectum empty into the portal venous system (by the sup. or inf. mesenteric veins, showing a similar pattern to the arterial supply).
The venous blood collected from the middle and lower thirds of the rectum flows into the internal iliac vein (through the middle rectal vein) and internal pudendal vein (through the inferior rectal vein), both veins drain their blood finally into the inferior vena cava. Therefore the area of the rectum (down to the haemorrhoidal zone) is an important border zone between the portal vein and inferior vena cava systems (containing one of the so-called portocaval anastomoses.
Another possibility to form such anastomoses between the inferior vena cava and portal vein systems occurs at the semi-intraperitoneal or completely retroperitoneal bowel parts where these organs have fused with the posterior abdominal wall: there is a possible way of venous drainage towards the posterior body wall also (these are the retroperitoneal anastomoses).
There are no valves in the mesenteric veins, therefore in case of increase in portal venous pressure (portal hypertension) certain symptoms, reflecting the difficulty of venous drainage can quite early occur. Administration of rectal suppositories in the lower part of the rectum has beneficial effects: the absorbed drugs of the suppository bypass the portal venous system and the liver, therefore the active agents get into the systemic circulation quickly and in higher concentration, so their use has faster and more powerful effects. In the venous plexuses of the rectum - probably due to the unhealthy, sedentary lifestyle the venous drainage gets less effective – haemorrhoidal nodes, "haemorrhoids" can often develop.
II./1.1.13.: The lymphatic drainage of the large intestine
The lymphatic drainage has high importance in the propagation of tumors or in their metastasis formation. Lymphatic drainage from the cecum, appendix, ascending and transverse colon leads into the mesenteric lymph nodes. Lymphatics from the descending, sigmoid colon and the rectum drain into the paraaortic lymph nodes. Lymph vessels coming from the transverse colon can also reach the pancreaticoduodenal lymph nodes and those located in the hilum of the spleen.
II./1.1.14.: The innervation of the large intestine
The large intestine is innervated both by extrinsic (sympathetic and parasympathetic) and intrinsic (plexuses of the enteric nervous system) nerves.
II./1.1.14.1.: The extrinsic innervation of the large intestine
|
 |
In case of the extrinsic innervation the left colic flexure – due to embryological reasons – signs an important boundary (called Cannon-Böhm’s point): the parts of colon situated proximally from this point receive their preganglionic parasympathetic innervation from the vagus nerve, while the distal parts of the colon are innervated by the sacral parasympathetic nerves (S2-4, pelvic splanchnic nerves). The synapse occurs mainly in the intramural plexuses located in the colonic wall; from there the relatively short postganglionic fibers reach the target cells (smooth muscle, glandular cells and immune cells).
The sympathetic nerves of the colon originate from the superior and inferior mesenteric ganglia and their postganglionic plexuses course to the target organ in the adventitia of the corresponding arteries.
The superior and inferior hypogastric plexuses contain a combination of both sympathetic and parasympathetic nerve fibers, delivering the extrinsic innervation to the abdominal and pelvic viscera.
The mechanism of pain perception: sensory receptors of the bowel wall are sensitive for strain, distension, increase of muscular tone. The viscerosensory nerve fibers conduct the pain sensation, having their perikarya in the appropriate dorsal root ganglion.
The innervation of rectum forms complex reflexes as well (for faecal storage or defecation), containing both autonomic and voluntary components. The centre of these reflexes is situated in the conus of the spinal cord, therefore lumbar spinal traumas may disturb the normal faeces and urine continence.
II./1.1.14.2.: The intrinsic innervation of the large intestine
The important components of the intrinsic innervation (enteric nervous system) are the nerve plexuses located in the intestinal wall, forming rich networks of nerve cells and fibers: the submucosal plexus of Meissner and especially the myenteric plexus of Auerbach. (The nerve plexuses of tela submucosa can be divided into at least two parts, according to the location of their neurons: the internal submucosal plexus [this is the Meissner’s plexus in narrow sense] and the external submucosal plexus [Schabadasch's plexus] can be distinguished.) In these plexuses different types of neurons are located (interneuron, sensory neuron, motor neuron). Not only the postganglionic parasympathetic neurons are found here, but also the nerve components of the local neuronal reflexes. The metabolism and biochemical composition of these neurons are different from those of the parasympathetic ganglion cells; can be fully functional also when separated from the parasympathetic nervous system.
Numerous specific molecules, acting as neurotransmitters and neuromodulators have been described in these neurons. In contrast to the small intestine the colonic motility, innervation and its neural reflexes are less well known. The absence of the ganglion cells of the intestinal wall (aganglionosis coli) results an extreme narrowing in the affected part of the colon (eg. in the rectum) in childhood - however the proximal part of the intestine dilates wide (the name of the disease refers to this symptom, not to the appearance of the affected part: megacolon congenitum, Hirschprung’s disease). The axons of motoneurons may arise from both plexuses of the intestinal wall (myenteric plexus, submucosal plexus). The neurons of the submucosal plexus are responsible for innervation of the circular muscle layer and the tunica mucosa (the latter ones can exhibit secretomotor or sensory fibers).
II./1.1.14.3.: Interstitial cells of Cajal
|
 |
More than a hundred years ago Ramon y Cajal described the intestinal interstitial cells, which were later named after him. Cajal characterized these cells as primitive "interstitial neurons" placed between the autonomic nerve endings and smooth muscle cells. During light microscopy, these cells were seen having processes (branching cytoplasm) and heterochromatic nuclei.
The interstitial cells form a complex network around nerve plexuses and smooth muscle cells. According to our present knowledge, these cells have non-neuronal origin (ie. not neurons or glial cells), but are derived from mesenchyme: modified smooth muscle cells which have lost their contractility. The interstitial cells occur in all parts of the gastrointestinal tract.
Synapse-like contacts with the nerve endings could be demonstrated and also very close appositions or gap junctions with the smooth muscle cells were detected. One group of the Cajal cells has a key role in mediating the inhibitory enteric innervation (neurotransmission) while the other subpopulation acts as intestinal pacemaker cells (basal electrical rhythm, "slow wave" generators).
In the large intestine the Cajal cells of the submuscular plexus (formed by interstitial cells, found at the inner side of the inner, circular muscle layer, facing the tela submucosa) are thought to have pacemaker function. Less literature data are available about the interstitial cells of the myenteric plexuses of the colon. It has been shown that the interstitial cells of Cajal are able to express the proto-oncogene KIT and its protein product (c-kit receptor, membrane receptor tyrosine kinase). The safest method to identify Cajal cells is the combined demonstration of their electrone microscopic characteristics and the c-Kit positivity.
|
|