
Observe the drawing!
|
III./1.2.: The wall structure of the stomach, Histology
The stomach exhibits the typical layered wall characteristics of the gastrointestinal tract (Illustration 3.). Its most important, most specialized layer is the relatively thick (2 mm) tunica mucosa.

Illustration 3: The histological structure of the corpus of the stomach. Observe the epithelial lining of the glands which is composed of different cell types (specific epithelium) !
|
III./1.2.1.: Tunica mucosa (mucous membrane)
The layers of the mucous membrane:
-
- epithelium mucosae,
-
- lamina propria mucosae,
-
- lamina muscularis mucosae.
Epithelium mucosae: the surface is covered by simple columnar epithelium called also surface mucous cells. These cells are characteristic secretory epithelial cells, producing mucus. Mucus makes a protective, thick, almost insoluble coating layer on the inner surface of the stomach (bicarbonate-rich "mucous barrier" against the self-digesting effect of gastric juice – since gastric juice is a very aggressive, highly acidic fluid having its pH about 1). The histological appearance of the surface epithelial cells can be characterized by their apical mucus droplets; the secretory vacuoles almost completely fill the cytoplasm. The mucus produced by them can be detected using mucus stainings (eg. with PAS staining they appear in purple colour).
Lamina propria mucosae: a loose connective tissue layer, into this the tubular gastric glands protrude. In the connective tissue lymphocytes, solitary lymphatic follicles and scattered smooth muscle cells can be found. The rich blood vasculature (arterioles, venules, capillaries) shows the importance of the blood circulation of the surface epithelium and of the glands (mucous membrane protection!).
Lamina muscularis mucosae: two layers of the well-developed smooth muscle belonging to the mucous membrane .
III./1.2.2.: Tela submucosa
A loose connective tissue layer, containing blood vessels, nerve cells and nerve fibers (submucosal plexus of Meissner). Numerous macrophages, mast cells and lymphocytes also occur in this layer. The tela submucosa of the stomach is always free of glands!
III./1.2.3.: Tunica muscularis propria
The own muscle layer of the stomach (Illustration 4.), composed of three sublayers:
-
- Oblique layer: the innermost, oblique smooth muscle layer; forming a single network between the cardia and fundus but more downwards is composed of rather radiating muscle bands.
-
- Circular layer: the circular smooth muscle layer of the stomach is present in all areas; strengthened around the cardia (here, however, there is no anatomical sphincter muscle) and in the pylorus (here, being rather strong, it forms the real pyloric sphincter muscle).
-
- Longitudinal layer: the outer longitudinal smooth muscle layer is especially pronounced along the curvatures.
Between the circular and longitudinal muscle layers the myenteric plexus of Auerbach can be seen, containing mostly multipolar neurons.
|

Observe the drawing!
|
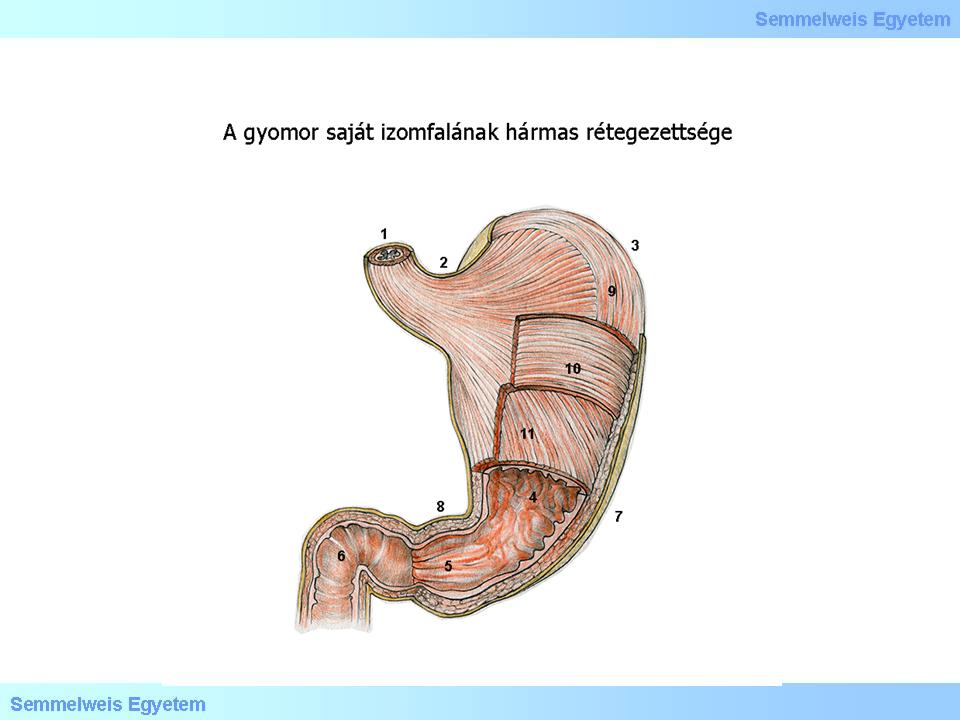
Illustration 4.: The own muscle layer of the stomach wall, exhibiting three sublayers
|
III./1.2.4.:Tela subserosa
Fatty connective tissue, containing larger blood vessels.
III./1.2.5.: Tunica serosa
The stomach, being a fully intraperitoneal organ, has a complete peritoneal covering. This layer is composed of a thin connective tissue (lamina propria serosae), followed by the outermost layer of simple squamous epithelium (mesothelium).
III./1.2.6.: Regional histological differences
|
 |
Above the previously mentioned general characteristics the mucous membrane exhibits regional differences. The glands differ histologically in the cardia, fundus, corpus and pyloric areas as follows:
III./1.2.6.1.: Cardia glands
Found in a 1-2 cm wide rim surrounding the esophageal orifice. Loosely arranged, sometimes branched tubular glands, which produce mucus, that’s why the secretory cells are stained pale.
III./1.2.6.2.: Fundus and corpus glands
The glands located at the fundus and corpus areas have the same characteristics and produce gastric juice for the digestion. Tubular glands, located parallel, extending into the lamina propria mucosae; more than one glands opening into one gastric pit . The depth of the gastric pits is about 1/3-1/4 of the thickness of lamina propria mucosae. Between the gastric pits the mucosal areas form the mucosal ridges (plicae villosae, villous folds).
The tubular glands have rather narrow lumen. Different parts can be distinguished in them: directly below their opening an initial constricted, narrow part (isthmus), below that the neck (cervix), after the body (corpus or principal part), finally the base (or fundus) at the bottom. At the cervix the mucus-secreting neck cells, sometimes parietal cells (producing HCl) and undifferentiated cells are located. In the corpus part of the glands the parietal cells predominate while in the base the chief cells are the most numerous. Enteroendocrine cells occur especially at the base area also.
III./1.2.6.2.1.: Mucous neck cells / mucus-secreting neck cells
The mucus-secreting neck cells are mucus producing cells occur in high amount at the cervical part of the glands (the mucus produced by them has a different composition than that of the mucus made by the surface mucous cells: acidic and less viscous). The irregular shaped cells have their nucleus at the basal part of the cytoplasm; many secretory granules are accumulated in the luminal part of their cytoplasm. Mucus produced by them can be visualized by mucus stainings (eg. with PAS staining they appear in purple).
III./1.2.6.2.2.: Undifferentiated cells
Located in the neck portion of the glands; with mitotic division they can replace the other cells. After the division the newly generated daughter cells move up or down in the epithelium to occupy the place of dead epithelial cells.
III./1.2.6.2.3.: Parietal (oxyntic) cells
These cells produce hydrochloric acid and intrinsic factor (a glycoprotein required for absorption of vitamin B12). They occur in the middle part (corpus) of the glands in large number, but can also be found at the neck and in the basal part. Large, round cells, having a central nucleus. Their –otherwise- pale stained eosinophilic cytoplasm appears in orange/red when using Congo-red staining. Only their narrow cytoplasmic process extending to the lumen is located between the other cells (such as neck cells), the majority of the cell is placed outside the row of cells bounding the lumen, somewhat like covering them (that’s why called "parietal cells"). They produce H+ and Cl- ions which unite outside the cells to form hydrochloric acid.
HCl activates pepsinogen into pepsin, and has also bactericid effect by killing bacteria arrived together with the food. The acidity of the gastric juice plays a key role in the gastric physiology and in the ulcerative and inflammatory diseases of the stomach as well. Using pharmacological intervention it can be reduced at several targets (eg. "proton pump inhibitors"). The parietal cells exhibit a typical, surface increasing intracellular canaliculus system, visible with electron microscopy.
Note that the hydrochloric acid and pepsin secreting areas (fundus and corpus) are surrounded proximally (at the cardia) and distally (at the pylorus) by "neutralizing" and protective mucus production zones.
III./1.2.6.2.4.: Chief cells (zymogenic cells)
Chief cells produce pepsinogen, stained basophil, seen especially in the base of the glands. Their basophil staining is due to their active protein synthesis (rER).
III./1.2.6.2.5.: Enteroendocrine cells
Enteroendocrine cells are hormone producing cells with round nucleus, found also at the basal portion of the glands, among the other epithelial cells; safely cannot be identified by light microscopy. Using electron microscopy the granules in the basal part of their cytoplasm can be observed. Exact identification is possible with immunocytochemistry. These cells are classified according to their hormonal product (G-cells: gastrin, EC cells [enterochromaffin cells]: serotonin, D-cell: somatostatin, ECL cells [enterochromaffin-like cells]: histamine, A cells: enteroglucagon etc.). Their hormone gets into the connective tissue of the lamina propria mucosae then to the neighbouring cells (paracrine function) or into capillaries (endocrine effects). Their physiological role (eg. in the regulation of the production of gastric juice) is very important. It is interesting that there are enteroendocrine cells emptying their secretion into the lumen.
III./1.2.6.3.: Pyloric glands
The gastric pits are deeper at this area than those seen in the fundus region, extending into the half, two-thirds of the thickness of lamina propria. Into these pits open the shorter, branching, tortuous pylorus glands. Their cells also produce protective mucus. The glands house many enteroendocrine cells (eg. gastrin-producing cells).
|
|