| |
IV./2.3.: Pathology of gastric ulcer
IV./2.3.1.: Etiology
IV./2.3.1.1.: Peptic ulcer (ulcus ventriculi pepticum)
|
| |
Peptic ulcers are produced by an imbalance between mucosal defense
mechanisms and damaging forces, particularly when the damaging effect of gastric acid and pepsin prevails. Internal defense mechanisms: mucus layer produced by gastric mucosal cells, bicarbonate ions, prostaglandins (PGI), and the epithelial cells itselves. External defense factors: medications with „mucosal coating” effect, nutrients with balancing effect and great protein content (dairy products), agents neutralizing hydrochloric acid (baking soda), etc.
Internal damaging factors: gastric acid, digestive enzymes (pepsin). External or pathological damaging factors: chronic gastritis (Micropicture 1 A-B.) caused by Helicobacter-pylori infection, non-steroid anti-inflammatory drugs (NSAID), alcohol, smoking, hyperacidity, gastroduodenal reflux, ischemia, shock, insufficient stomach exhaustion, hot, spicy diet, acid and alkaline agents).
The ulcer develops at the weakest point(s) of the mucosa (locus/loci minoris resistentiae), namely at the location(s) of the above mentioned imbalance, thus it can have one or multiple foci.
|

Study the pictures!
|
Micropictures 1 A-B: Helicobacter pylori bacteria – rod and less common spherical forms – can be detected with special hystochemical (A) and immunhystochemical (B) methods (A: Warthin-Starry stain; 400x; B: H. pylori; 600x). (Source: Semmelweis University 2nd Department of Pathology, collected by István Kenessey)
Peptic ulcer develops mostly in middle-aged or elderly men (gastric ulcer’s sex distribution ratio is male:female=2:1). Gastric ulcer is accompanied by duodenal ulcer in 10-20% of the cases, however – due to the duodenal presence of the acid-peptic stomach content – duodenal ulcer is often develops by itself. Sex distribution ratio of duodenal ulcer is male:female=3:1. Thus the most common location of the peptic ulcer is the stomach or the duodenum, but it can develop also at other locations, where, due to the presence of ectopic or metastatic gastric mucosa islands, conditions for its formation are met: in the esophagus (on the grounds of Barrett-metaplasia), or in the Meckel-diverticulum (on the grounds of gastric mucosa ectopy).
As for the macroscopic appearance of gastric ulcers, they typically have a punched-out, regular roundish-oval shape with straight, exquisite walls (Macropictures 1A-B.). Walls can be rampartlike swollen due to the perifocal mucosal oedema, but this oedema never reaches the size of the tissue proliferation surrounding the malignant ulcers (see there). Base of the ulcer can be hemorrhagic, more often it is covered by debris and fibrin coat. After a few days it becomes granular due to the several vascular buds sprouting from the ulcer base in the course of granulation, an important phase of wound healing. Granulation tissue is named after these vascular buds or tiny, grain-like (granular) sprouts.
|

Study the features in the pictures!
|
1A-b macropictures: Ulcus acutum ventriculi. Both pictures show an actively bleeding ulcer. A: Besides the ulcer in the foreground of the left picture, two other, smaller ones are present (a bit to the upper left). These three lesions can almost be fitted to a straight line: this is a typical location for ulcers developing on the longitudinal mucosal folds of the small curvature.
After a while – within several weeks – , due to the activity of the fibroblasts that migrated here, the granulation tissue becomes richer in collagen fibers, less rich in veins and leukocytes, and slowly turns into scar tissue. This transformation has a typical direction: it occurs from the deep layers towards the surface, thus from the outside towards the lumen the following layers can be differentiated:
(a) the oldest layer is located at the bottom, this is the first to turn into scar tissue,
, thus this is the scarry base of the chronicized ulcer, its thickness gradually increases towards the lumen by time;
(b) inflammatory granulation tissue zone, rich in veins and cells, this is the ulcer’s real frontline: its bottom line - due to the above mentioned collagen fiber production - gradually merges into the scarry ulcer base, while its upper margin merges into the next layer on its surface, because the new sprouting vascular buds grow into the more superficial layers of this zone and annexes it into the granulation tissue zone (this process is called organization);
(c) superficial zone with debris and inflammation, this constitutes the visible surface of the ulcer, and it consists of precipitated fibrin (inflammatory exudate), inflammatory cell elements and the residuum of the original tissue parts.
From its bottom, the approaching frontline of the granulation tissue gradually annexes this zone, thus by time it also turns into granulation tissue, which turns into scar tissue. This way the organization of the ulcus becomes complete, and chronic ulcer develops, which is a scar tissue that replaces ruined wall elements and restores tissue incontinuity in the mechanical aspect (Macropicture 2.)
|

Study the picture!
|
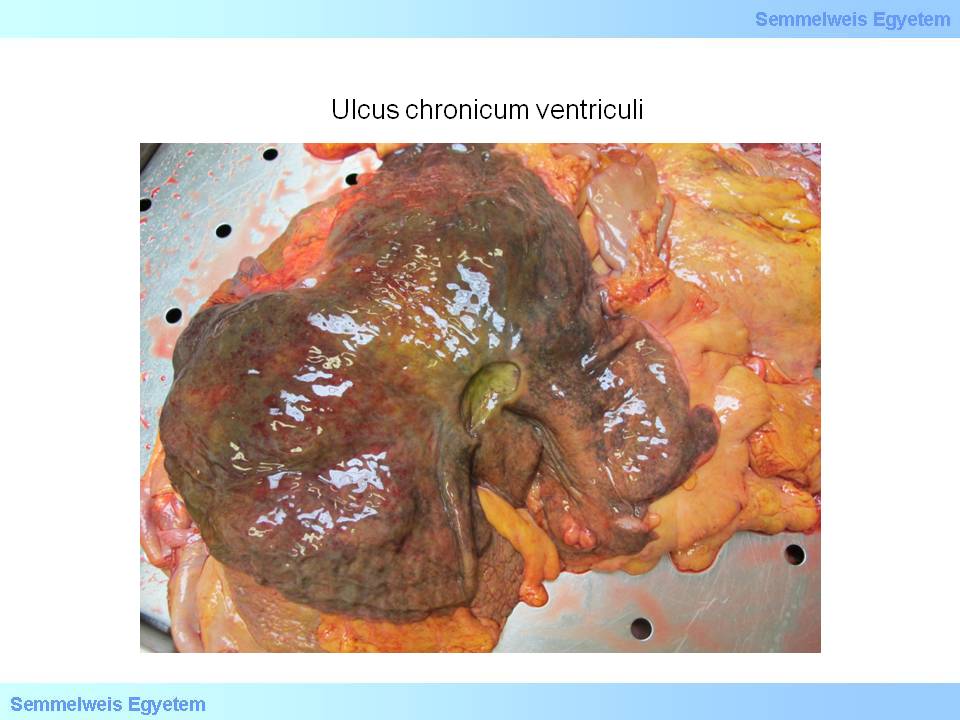
Macropicture 2: Ulcus chronicum ventriculi. Crater-like gastric ulcer, recovered with scar tissue at its bottom. (Source: Semmelweis University 2nd Department of Pathology, collected by Attila Kovacs and Ildiko Szirtes)
|
Note that there are multiple metastases in the liver piece on the right side of the picture. As judged by their appearance the presented gastric ulcers
are not tumor-induced, rather peptic (compare the cauliflower-like tumor increment on Picture 3. with the mainly flat ulcer form here with only perifocal oedema), we can assume that in this case ulcer is only co-occurring with the tumor and basically caused by stress. These ulcers – as shown by the black, coffee grounds-like, coated ulcer base – can also bleed just like primary peptic ulcers, and they can even cause the cancer patient’s death . (Source: Semmelweis University 2nd Department of Pathology picture archives, collected by Attila Kovacs and Istvan Kenessey) B: In the picture on the right, the ulcer developed also in this typical location, the antrum-corpus border of the small curvature. A usurated vein intersect can be found on the ulcer base. The bleeding leading to the patient’s death originated from here. (Source: Semmelweis University 2nd Department of Pathology picture archives, collected by Attila Kovacs and Ildiko Szirtes)
|

Study the main points of the picture!
|
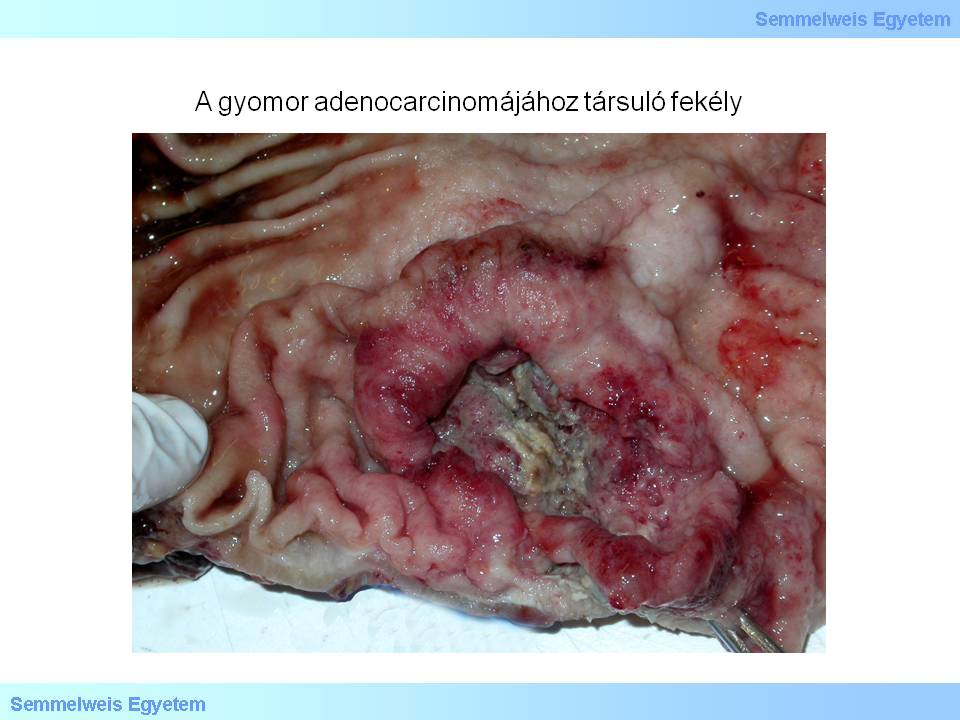
Macropicture 3: Ulcer associated to gastric adenocarcinoma. This macroscopic appearance is typical of the interstitial tissue type tumors, however, it is notable that the two basic tissue types (interstitial and diffuse) can be present even within the same tumor: namely by progressive dedifferentiation the glandular interstitial type can turn into the diffuse type which does not follow any tissue structure just spreads in the form of discohesive mass of sparse cells (Source: Semmelweis University 2nd Department of Pathology picture archives, collected by Attila Kovacs and Istvan Kenessey)
|
The most common cause of the gastric ulcer is the chronic gastritis caused by Helicobacter pylori (H. pylori) (Micropicture 2.) Warren JR Australian pathologist noticed in the beginning of the 1980s, that by then unknown, spirallic bacteria can be detected in 50% of the tissue samples originating from the antrum canal of ulcer patients. His colleague, Marshall BJ succeeded in breeding the bacteria. Thus they were the first to show that there is a connection between H. pylori infection-induced chronic gastritis and the development of gastric and duodenal ulcer. The researchers proved their hypothesis with self-experimentation (self-infection) and several further studies. It was their scientific work that led to the treatment of ulcer disease, thus they deservedly received the medical Nobel-prize in 2005 as a reward for their work.
|

Study the details of the picture!
|
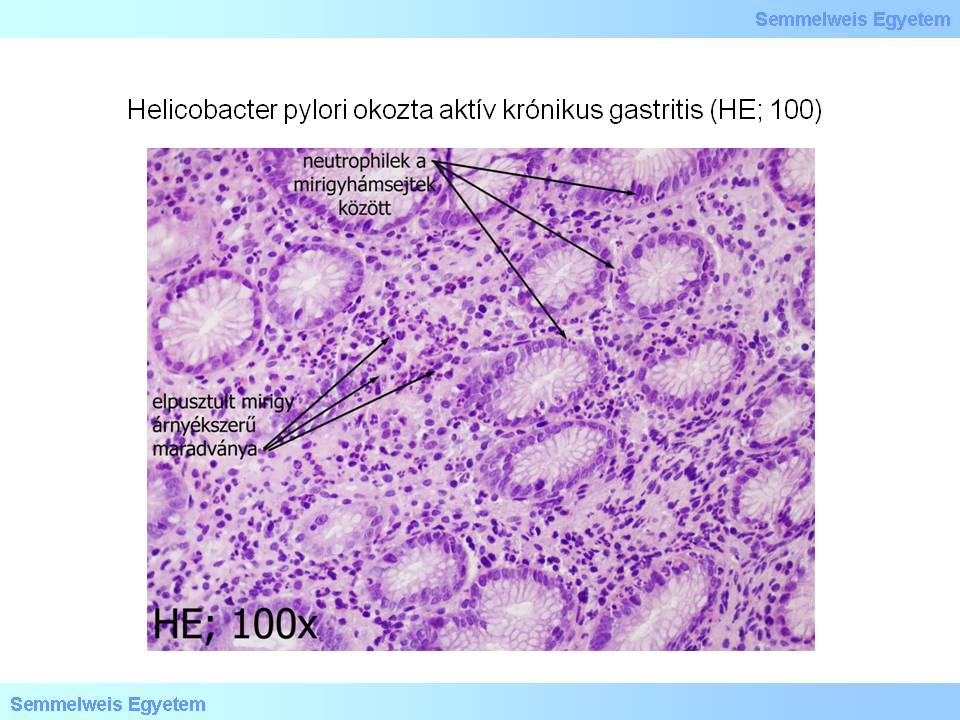
Micropicture 2: Active chronic gastritis caused by Helicobacter pylori. Bacterial colonization of the mucosa is relatively consistently associated with the activity signs of chronic gastritis, which means that neutrophil cells mix with the otherwise typically lymphocytic stroma infiltration, and these penetrate between the epithelial gland cells. If severe inflammation exists for a long time, it eventually leads to glandular destruction (see the picture!) and thus atrophic gastritis. In another appearance form of the atrophic gastritis the number of glands and the thickness of the mucosa does not decrease significantly, but the specific epithelium of the glands decays, and this epithelial layer that normally includes the symbiotic group of several cell types is replaced by foveal epithelium that contains only one cell type (HE; 100x) cells (Source: Semmelweis University 2nd Department of Pathology, collected by Ildiko Szirtes)
|
The micro-organism belongs to Proteobacteria phylum, epsilon Proteobacteria class, Campylobacterales order, Helicobacteraceae family, Helicobacter genus. It is a Gram-negative, flagellar, microaerophil, curved rod or helix-shaped, motile bacteria, with 2-3 micron length, 0,5-1 micron diameter, and 1-7 lophotrichous flagella. One of its enzyme products is the urease that hydrolyzes urea to ammonia and bicarbonate, thus neutralizing the acidulous microenvironment unfavorable to the bacteria. The urease enzyme allows bacterial colonization in the superficial layers of the gastric mucosa that were traditionally thought to be sterile. The ammonia breakdown product has a direct cytotoxic effect, too. In addition, the bacteria increases the production of membrane destructive enzymes (e.g. phospholipase A, C), and being a foreign micro-organism, it attracts inflammatory cells (neutrophil granulocytes) to the site, from which myeloperoxidases, reactive oxygen species are released, also damaging the epithelial cells of the mucosa (called active chronic gastritis)
H. pylori infection affects more than half of the world population. Nearly 65% of the Hungarian adult population is infected with the bacteria and in approx. 15% of the infected population ulcer is formed. According to current knowledge, H. pylori can only spread from person to person, animal or other natural reservoir has not been found yet.
According to the epidemiological studies, the route of infection is faecal-oral and generally occurs in early childhood. There are significant differences between developing and developed countries’ epidemiological data. In developing countries, 80-90% of the adult population is infected, while in developed countries only approx. 20% of the people under the age of 40 carry the bacteria. The development and clinical course of H. pylori-associated diseases is influenced by the age of acquiration. The longer the time of the bacteria carrier status, the greater the risk of subsequent gastric and duodenal mucosal lesions.
IV./2.3.1.2.: Iatrogenic (postoperative) ulcer (ulcus iatrogenicum)
Any kind of major surgical intervention may lead to post-interventional stomach ulcer, so this form is actually related to stress-related ulcer. In a narrower sense, in terms of gastrointestinal surgeries, the altered post-operative anatomical situation itself can lead to peptic ulcer at otherwise unusual places: ulcers in the jejunum are not uncommon after Billroth II. gastric resection (resectio ventriculi), as in these cases stomach contents directly (i.e., without dilution) contact the jejunal mucosa in great amount and thus become a damaging factor.
IV./2.3.1.3.: Cancer-related ulcers (ulcus ventriculi propter tumorem)
Both benign and malignant tumors of the stomach mucosa or deeper wall layers can be associated with ulcer as an accompanying symptom (Macropicture 9P-3.) Real mucosal polyps’ surface can ulcerate due to the acid-peptic environment, their roundup into the lumen and their mechanical-chemical contact with the food content. The prolipherating surface of larger adenomatosus polyps can be fragile and become ulcerated on circulatory-nutritional basis. Mucosal ulceration can also occur on protuberating surfaces of submucosal, mesenchymal tumors, e.g. on polyposus, protuberating submucosal lipomas, leiomyomas or intramural GISTs (gastrointestinalis stromalis tumor) that grow towards the lumen.
The ulceration of the stomach cancer sprawl is a common phenomenon: mainly the cauliflower-like flatly protuberating mass of so-called intestinal tissue type cancers ulcerates in a crater-like form. The other tissue type (the so-called diffuse tissue type) stomach cancers – typical example of which is the signet ring cell carcinoma (carcinoma sigillocellulare) typically and primarily grow towards the depths of the wall and thicken the deeper wall layers while leaving the mucosal surface hardly affected or almost intact – this is the macroscopic picture of linitis plastica (Macropictures 9P-4A-B.)
The macroscopic appearance of cancer, due to the autonomous tumor proliferation, is characterized by gnawed, irregularly rampart-like margins and on this basis typical tumor ulcers can be differentiated form peptic ulcers.
|

Study the pictures!
|
4A-B macropictures: A.Typical appearance of diffuse tissue type stomach cancer: the ever-increasing space-occupying mass thickens and stiffens the submucosal wall layers under the intact mucosa. Although this type – similarly to the intestinal type – originates from the glandular epithelium of the mucosa, its growth is mainly infiltrative and inward-spreading.
During a gastroscopy, especially in the early stage of development, it can escape the attention of the examiner, as only the slight smoothing of the mucosal folds and the local shortfall of the peristaltic wall motion can indicate the deep underlying process. If sampling biopsy is done, sometimes it only contains intact mucosa.
B: According to some sources, the name of the growth form typical of the diffuse type stomach cancer – linitis plastica – originates from the English word „linen”, because the thickened gastric wall reminded the old English pathologists of the freshly washed and ironed linen’s crispy firmness, and misinterpreting they saw the essence of the disease in the gastric inflammation. Thus they created this unusual neology by completing the word „linen” with the Latin ending for inflammation. (Source: Picture Archives of Semmelweis University 2nd Department of Pathology, collected by Ildiko Szirtes and Attila Kovacs)
IV./2.3.1.4.: Stress-related ulcer
|
 |
Peripheric vasoconstriction and microcirculatory disturbance caused by an increase in sympathetic tone stands in the background of its development, due to which relative hypoxia occurs in the concerned mucosal areas, making their cells vulnerable. Furthermore, cells become unable to produce and reproduce the important chemical elements of the protection (particularly the covering mucous film). Therefore the damaging factors’ dominance develops and a patogenetically typical peptic ulcer evolves. Its formation is typically present as a concomitant phenomenon of life-threatening diseases of large, parenchymal organs (heart infarct, stroke – the ulcus associated with the latter is called Cushing-ulcus); as a complication of big traumas (the so-called Curling-ulcus), long and demanding operations, advanced tumors (Macropicture 9P-1A), or associated to stressful, perfectionist lifestyle (so-called manager-disease).
IV./2.3.1.5.: Ulcer with endocrine origin (Zollinger-Ellison-syndrome)
The pathological hormonal environment in this disease also leads to ulcers. Multiple ulcers develop in the stomach, duodenum and even in the jejunum, often with much greater size compared to usual peptic ulcers (so-called giant ulcers).
The disease is due to a gastrin-producing one or multifocal, pancreatic, less often gastric or intestinal cancer (so-called G-cell APUDoma).
The three main characteristics of Zollinger-Ellison syndrome: 1. Significantly increased gastric acid production and gastric musocal hyperplasia with giant folds (gastropathia hypertrophica), 2. Giant peptic ulcers, 3. neuroendocrin tumor of one of the above mentioned organs. The latter is malignant in half of the cases and forms most commonly liver metastases. The syndrome most commonly occurs between the ages 40-75 years, it is 1.5 times more frequent in males than in females and 20% of the cases are associated with MEN-1 syndrome. Clinical signs: 1 abdominal pain (especially in the upper abdomen), 2. vomiting refractory to conventional drug therapy, 3. esophagitis (due to the regurgitation of acidulous stomach contents), 4. diarrhoea, 5. ulcers not responding to conventional drugs, 6. weight loss.
IV./2.3.2.: Morphological characteristics
IV./2.3.2.1.: Erosion
By definition, erosion isa breach in the mucosa which does not spread deeper than the lamina muscularis mucosae (Macropicture 5.)
|

Study the pictures!
|

Macropicture 5: The larger lesions are ulcers. Next to them, the several, point, scattered, dark purple, superficial breaches are erosions. Their colour indicates that both the ulcers and the erosions bleeded actively (Source: Picture Archives of Semmelweis University 2nd Department of Pathology, collected by Istvan Kenessey and Attila Kovacs)
|
Despite being superficial, erosions can bleed from the mucosal capillary network, and as erosions are usually multiple and they can be present in even very high numbers in the gastric mucosa, these multiple tissue breaches altogether can cause significant blood loss that destabilizes the whole circulation (so-called shock-inducing bleeding), even though only a small amount of bleeding comes from each erosion. At the same time, due to their superficiality, their prognosis is very good, under favourable conditions they can crust within a few hours.
Their macroscopic appearance is characterized by small (about 1 mm in diameter), point-like, regularly roundish indentation on the mucosal surface, which is most visible during an autopsy if the examiner lifts the mucosal area in question to eye level and lets the incident beam sparkle on the mucosal surface; erosive breaches are easiest to spot on the luminous surface. This way even the slight, rampart-like circular musocal swelling, that accompanies the erosion as perifocal oedema, becomes visible. If the erosion bleeds actively, its location is also indicated by the adherent black precipitation (acid-haematin) in the mucosal dells, which is the residue of the blood digested by hydrochloric acid, non-washable under light jet.
IV./2.3.2.2.: Ulcus (ulcer)
By definition, an ulcer (ulcus) is a deep mucosal breach, which spreads deeper than the layer lamina muscularis mucosae, namely minimally reaches or spreads beyond the submucosa (Micropictures 3-4.) Its horizontal size is also greater than that of an erosion: they are commonly 0.5-2 cm in diameter, but bigger ulcers can occur.
|

Study the pictures!
|
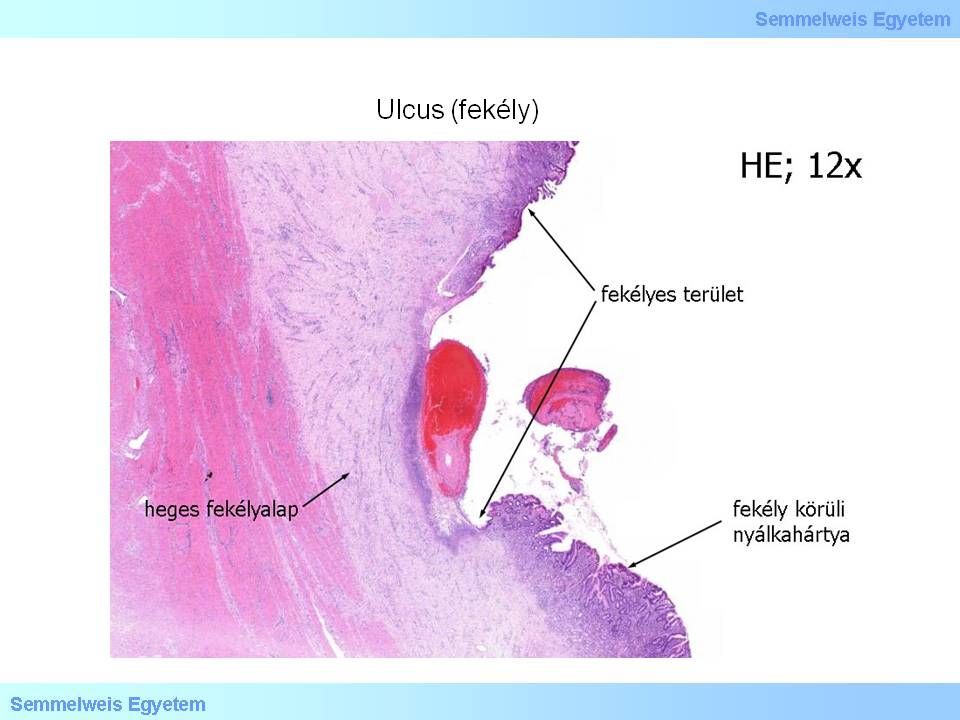
Micropicture 3:A scarry ulcer base is present under the thin granulation layer in chronic ulcer (HE; 12x). (Source: Picture Archives of Semmelweis University 2nd Department of Pathology, collected by Istvan Kenessey)
|
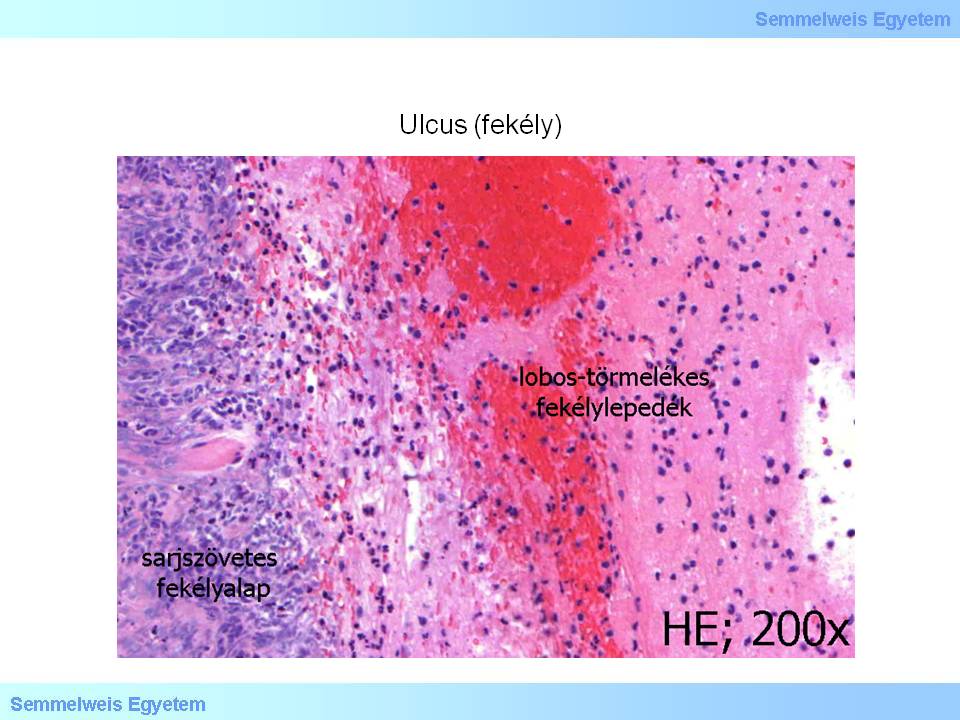
Micropicture 4: The base of the acut ulcer consist of vascular and cellular inflammatory granulation tissue (see left side of picture), which is covered by structureless ulcer coat. The latter consist of tissue debris, inflammatory cells and fibrin network (HE; 200x). (Source: Picture Archives of Semmelweis University 2nd Department of Pathology, collected by Istvan Kenessey)
|
IV./2.3.2.3.: Perforation (transfixion)
If the tissue breach caused by the ulcer is so deep that it pierces through all the wall layers, a transmural lesion, a real, open transfixion (perforation) can occur. It can be interpreted as a morphological variant of ulcer (perforated ulcer), but also as its complication. By its development, stomach content gets into the free abdominal cavity, and due to both its chemical (acid pH) and biological (infectious agent content) characteristics causes an inflammatory reaction and fibrinous-purulent exsudation on the surrounding peritoneal surfaces (peritonitis acuta fibrinoso-purulenta).
From the stomach air sac, air pockets are formed in the free abdominal cavity. This can be easily detected by imaging techniques and is a typical radiodiagnostic sign of gastrointestinal perforation. The initially circumscribed peritonitis (peritonitis circumscripta) can later spread to the whole abdominal cavity, evolving to a generalized peritonitis (peritonitis generalisata) and ultimately leading to acute abdomen.
IV./2.3.2.4.: Penetration (closed transfixion)
In cases with benign prognosis, another organ or organ part can cover the hole of the perforated ulcer on the outer surface. In this case we are talking about a closed perforation, also known as penetration. This development prevents the complications mentioned at the open perforation, thus this can be considered as a kind of spontaneous recovery mechanism or a variant with favourable prognosis. The inflammatory reaction developing around the wall defect, primarily the produced exudate behaves like an adhesive and at first sticks the foreign organ on the peritoneum surrounding the penetration, then with the organization of the exsudate this adhesion evolves into an inseparable callused concrescence.
Organs that cover gastric perforation from the outside are most commonly the liver, the pancreas and the mesentherium. Penetration can also be considered as a morphological variant of ulcer (penetrating ulcer), but it can be understood as a complication, similarly to perforation. The word „penetration” comes from the fact that the adjacent, covering organ is never left untouched by the inflammatory processes of the perforation as these spread into the covering organ to some extent, that is, pierces through, penetrates into it. The consequentive cicatrisation also appears in the adherent organ’s parts that are next to the penetration, and the penetrated wall parts coalesce here with the organ stuck from the outside. The presented dissection is a demonstrative example of this phenomenon.
|
|