 |
II/2.3: Endocardial inflammatory diseases (endocarditis)
II/2.3.1: About inflammatory cardiac diseases in general
In part of the cases, endocardial membrane inflammations are indeed confined to the endocardium, but other structures of the heart might also take part in the inflammation – the musculature as myocarditis, the pericardium as pericarditis – and it leads to an extended cardiac inflammation (pancarditis). Endocarditises include inflammation of parietal endocardium (parietal endocarditis) and valvular endocardium (valvular endocarditis) – the latter being the most important endocarditis group.
II/2.3.2: Infective endocarditis
II/2.3.2.1: Incidence
The risk of endocarditis is increased in patients who live with any morphological valvular anomaly or deformity of any origin:
|
 |
-
1. chronic rheumatic/degenerative valvular deformities (microscopic image No.1),
-
2. congenital valvular heart diseases,
-
3. artificial valve implant (valvular prosthesis).
It is also a risk factor if the pathogens can enter the blood flow through a non-physiological, direct route:
-
4. under iatrogenic circumstances, e.g. in case of permanent catheter used for pain management in cancer patients, or
-
5. in case of intravenous drug users (cca. 15% of the cases), when endocarditis typically affects the tricuspid valve which is not the ordinary localisation.
|

Study the image and analyze what you see!
|
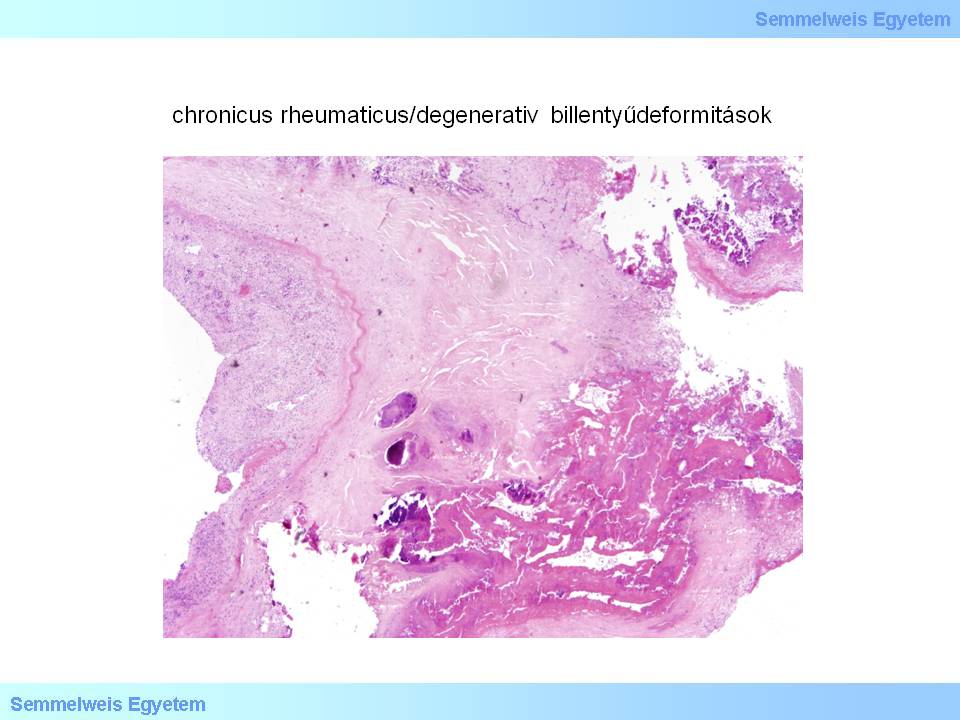
Microscopic image No.1: (HE; 40x) Scarred-calcified thickening of the valvular tissue represents the baseline valvular deformity, while granulation tissue formation seen on the left side is a consequence of acute exacerbation. (From the collection of the 2nd Institute for Pathology, Semmelweis University – collected by István Kenessey).
|
II/2.3.2.2: Pathogens
|
 |
They are almost always bacteria – Staphylococcus auerus, Streptococcus viridans, Gonococci, Enterobacteria; and so-called opportunist bacteria in immunodeficiency. Fungi also may cause endocarditis rarely, under special circumstances, for instance in immunodefficiency (see AIDS) or in intravenous drug users.
II/2.3.2.3: Clinical picture
|
| |
Acute and subacute manifestation forms are clinically different. Acute endocarditis is characterized by sudden onset, high fever, and septic crisis, and the patients appear very sick. In spite of antibiotic use, this form has a very high mortality. The subacute form (subacute infective or slow or malignant ulcerative endocarditis) starts with a latency and over a longer period with usually insignificant, general symptoms (weakness, fever, weight loss). In this underhand form it is not obvious how severe the patient’s condition is.
Emboli might be swept of from the vegetations that form on the valves, and they can create the clinical image of Schottmüller’s triad: endocarditis, splenic infarctions and embolic focal nephtritis. Osler’s node is a pathognomonic phenomenon which is a livid, painful swelling on the fingers’ distal phalanges and soft tissue around the nails, caused by (micro)embolisation originating from the endocarditis vegetations. The most severe complication of the disease forms when the whole blood path gets infected from the valvular appositions continously and over a long time, and it leads to blood flow infection (sepsis).
II/2.3.2.4: Morphology
Morphological appearance is similar in the two forms, therefore the acute and subacute variations can’t be told apart on morphological basis. The most important and most typical alteration in both forms is the appearance of valvular appositions (vegetations) on the cusps’ closing edges. The size of these vegetations may range from small granular appositions to large polypoid, narrowing vegetations. The substance of these appositions is crumbling, thrombotic-necrotic, inflammatory exudate debris including a large amount of pathogens (so-called bacterial clouds). The risk of embolisation from this infected and crumbling substance is great. If such an embolus gets stuck in a narrow section of the peripheral vascular system it will become a new infective focus itself, and may be the origin of a steadily growing inflammatory response susceptible of organization. Such abscesses that form at a new site further away are called metastatic abscesses.
|

Read the reference!
|
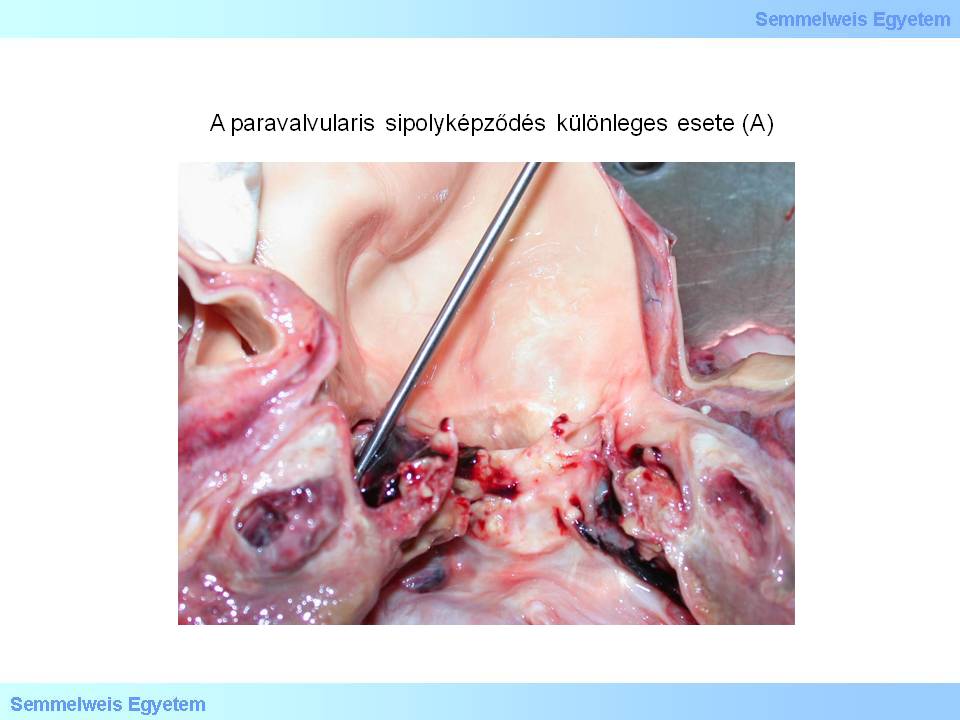
The valvular tissue gets damaged by necrosis, ulceration (macrosopic image No.1) and thrombus formation (malignant ulcerative endocarditis), and the valve which was weakened by inflammation often bulges and thus a so-called valvular aneurysm forms. Inflammatory destruction may even lead to valvular rupture (macroscopic image No.2A-B) and thus a sudden onset valvular insufficiency develops. Tissue destruction can extend to the neighbouring parts of the aorta or myocardium and a so-called paravalvular abscess (macroscopic image No.3A), paravalvular leak (a fissure or fistula along the valve) might form which serves as a break-out site for the high pressure blood flow. This is practically a circulatory catastrophe situation, because inflammatory paravalvular fistulae might open to the pericardial sac, and this leads to pericardial blood effusion (hemopericardium) and pericardial tamponade.
|

Study the image and analyze what you see!
|
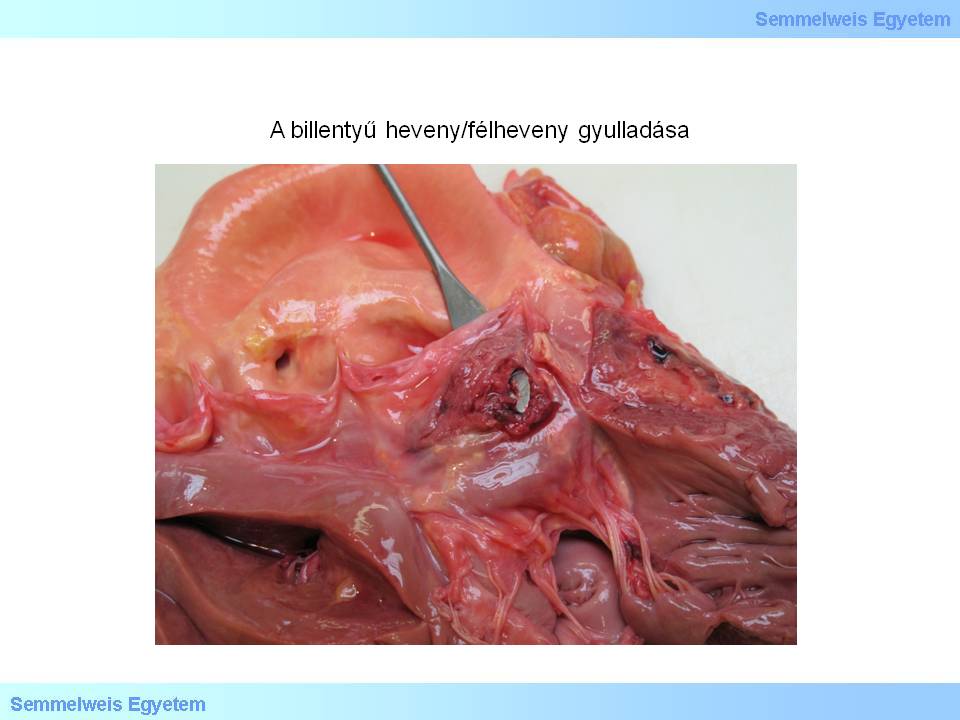
Macroscopic image No.1: Acute/subacute valvular inflammation led to cusp destruction which extended to the myocardium directly neighbouring the valvular basis. Two small holes are seen under the free edge of the valve on the left and right side. This is the typical manifestation of fenestrated valve (also see macroscopic image No.2P-9) (From the archives of the 2nd Institute for Pathology, Semmelweis University – collected by Attila Kovács and István Kenessey).
|
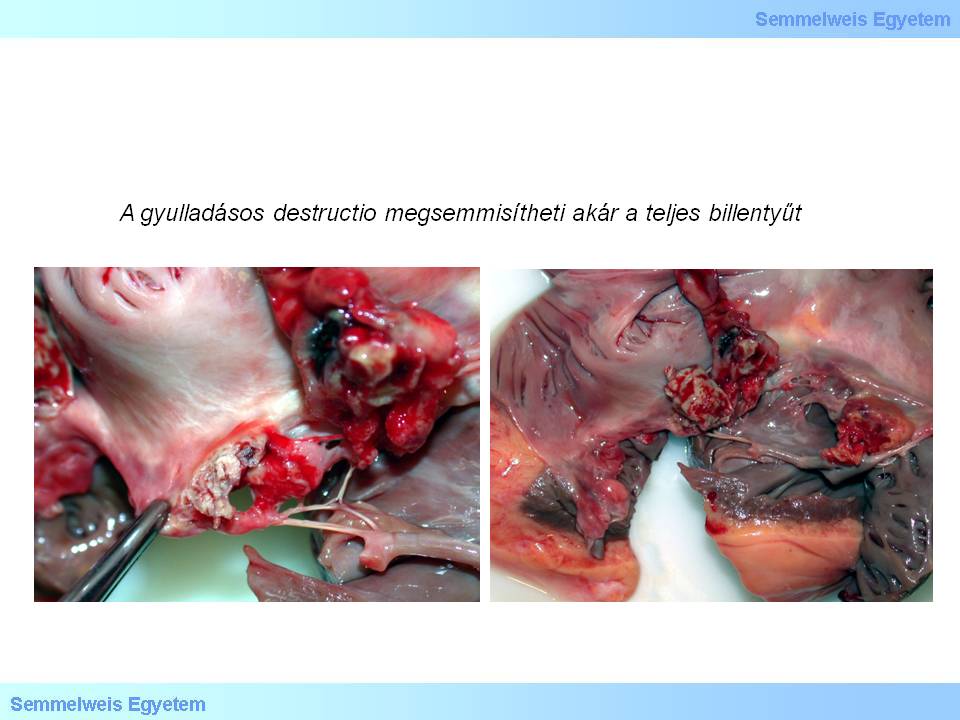
Macroscopic images No.2A-B: Inflammatory destruction may destroy the whole valve or lead to valvular rupture (From the archives of the 2nd Institute for Pathology, Semmelweis University – collected by Attila Kovács and István Kenessey).
|
 |
 |
Macroscopic images No.3A-B: A special case of paravalvular fistula formation: The path starts from the abscess behind the right aortic valve cusp (A) and through the muscular arch separating the right ventricle’s inflow and outflow tract (supraventricular crest) it leads to the right ventricle (B). A: The image shows subacute destructive endocarditis which is the antecedent of this process, and which developed on the grounds of chronic calcified valvular deformity. Observe the paravalvular abscess which developed in the angle formed by the aortic root and the upper end of the myocardium, in the subepicardial fat tissue. The probe bobbing up from behind the right valve cusp marks the location of the upper, aortic end of the fistula. B: the shaft of the probe is seen inserted in the lower, right ventricular end of the fistula path, and large amount of granular tissue proliferates around it (From the collection of the 2nd Institute for Pathology, Semmelweis University – collected by Tibor Glasz).
If the paravalvular abscess forms in the virtual space between the aorta and truncus pulmonalis, the developing fistula path will break in the right ventricle’s outflow tract instead of the outside world (macroscopic image No.3B). In this case a bidirectional regurgitation flow develops: on the one hand toward the left ventricle through the destructed aortic valve, and on the other hand toward the right ventricle through the fistula. This can be well detected with echocardiography. In severe cases endocarditis may spread to the tendinous cords, the parietal endocardium, that is, primarily valvular endocarditis becomes chordal or parietal and vice versa: primarily parietal endocarditis can become complicated by a valvular component.
Acute/subacute valvular diseases lead to acute and severe load of the affected ventricle, and cardiac failure develops rapidly, which is dominated by ventricular dilation and even ball like expansion. If significant ventricular hypertension is also present in the same time, it indicates prolonged ventricular load and that some chronic form of valvular heart disease was present before the acute disorder, e.g. rheumatic valvular disease. (Ventricular hypertrophy without dilation is called concentric hypertrophy; ventricular hypertrophy with dilation is eccentric hypertrophy.) Following artificial valve implantation, sterile or infected inflammation might occur on the artificial valve structures, this is called prosthesis endocarditis. Appositions often form along the artificial valve sutures, and complicated paravalvular abscess and leakage are also frequent.
II/2.3.3: Rare forms of endocarditis/ noninfective endocarditis
II/2.3.3.1: Non-bacterial thrombotic endocarditis
(macroscopic images No.4A-B). In this form small sterile fibrin and platelet vegetations appose in the closing edge of the valves. Its reason is often increased blood clotting tendency in seriously ill patients in poor general condition (end-stage tumour, chronic renal failure, chronic sepsis).
|

Study the images!
|
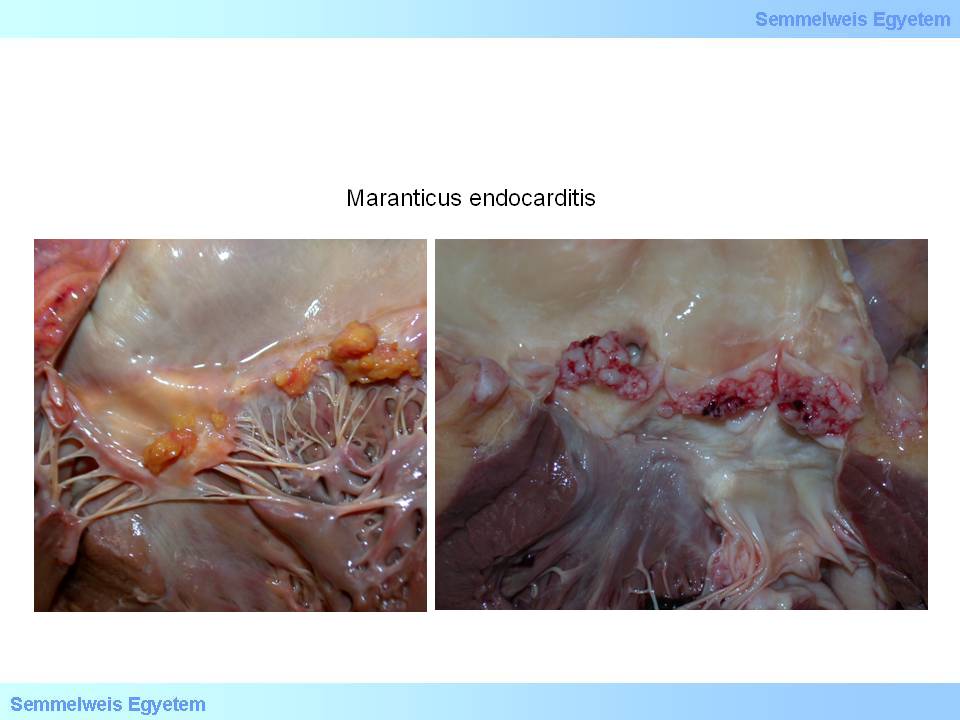
Macroscopic images No.4A-B: Marantic endocarditis. The irregular sized appositions consisting of platelets and fibrin fibers are sterile, and are close to the closing edge. Their developement is suggested to be the result of coagulation balance crush in seriously ill and dying patients (From the archives of the 2nd Institute for Pathology, Semmelweis University – collected by Attila Kovács and István Kenessey).
|
II/2.3.3.2: Libman-Sacks endocarditis (SLE-endocarditis)
It is an atypical verrucous endocarditis, where sessile appositions of 1-4 mm form mainly on the closing edge or lower surface of the posterior cusp of the mitral valve. Histologically it is characterized by fibrinoid necrosis, and later by fibrosis, valvular deformity and valvular heart disease. Histologically so-called hematoxyphil bodies are seen.
II/2.3.3.3: So-called carcinoid-endocarditis
It acccompanies neuroendocrine tumours (previous name: carcinoid) that develop in the gastrointestinal system (appendix, duodenum). The lesions mainly form on the tricuspid valve, and the cusps of this valve thicken like a glass. Similar lesions may occur on the pulmonary valve cusps, on the right ventricular endocardium, and in the truncus pulmonalis. This phenomenon is caused by direct effect of the tumour’s products with strong cardiovascular effect on the endocardial surfaces. Venous blood flowing into the right ventricle contains large concentrations of serotonin, kallikrein, bradikinin, histamin, prostaglandins, and tachikinins. The vast of these substances decompose while pass through the pulmonary circulation, and therefore they don’t harm the left ventricle’s endocardium.
II/2.3.3.4: Postinfarction endocarditis
|
 |
The most common non-infective endocarditis form which develops after acute myocardial infarction, usually in a parietal localization, and directly above the necrotized myocardium.
II/2.3.3.5: Syphilitic/luetic endocarditis
It is caused by luetic aortitis spreading to aortic valves. The valves get thickened and rigid, and in the late stage the valves become insufficient.
II/2.3.3.6: Rheumatoid arthritis (primary chronic polyarthritis – PCP) associated endocarditis
The alterations are ssimilar to what’s seen in luetic valvulitis.
|
|