|
I./2.3.: Complex urological deformations, related abnormalities
I./2.3.1.: Sacculated kidney (hydronephros, hydronephrosis)
|
 |
The urinary outflow can be inhibited by morphological or functional abnormalities of the urinary tract (so-called obstructive uropathy). Morphological abnormalities include strictures and obstructions. They can develop slowly or quickly as well. Sudden obstructions – if they are unraveled surgically or by themself (e.g. after a kidney stone attack) – are not leading to permanent complications. On the contrary, in case of slowly developing and permanent strictures the pressure of the urine above the obstruction is increasing, which leads to a dilated ureter (hydroureter), and also to the dilatation of the renal pelvis and calices (hydronephrosis); the latter one is accompanied by the pressure atrophy of the renal cortex (compression atrophy).
Causes of a unilateral hydronephrosis: stone in the ureter (ureterolithiasis), blot clot (e.g. injury of the renal pelvis or ureter due to a kidney stone attack), renal papillonecrosis, tumour of the ureter (transitional cell carcinoma, leiomyoma, etc.) (1st macropicture), ureteral stricture (congenital ureteropelvic junction obstruction, or acquired strictures, e.g. due to scarring), ureteral kinking (too long ureter due to a developmental malformation, or due to a constitutional ’floating kidney’, the so-called renal ptosis), or outer strangulation or compression of the ureter (fibrosis in the lesser pelvis, e.g. after cervical or endometrial cancer radiotherapy, etc.; periureteral tumorous invasion in case of a regional tumor – e.g. rectum carcinoma; iatrogenous, accidental ligation during – e.g. gynaecological - surgery in the region).
|

Look at the picture and analyze it!
|
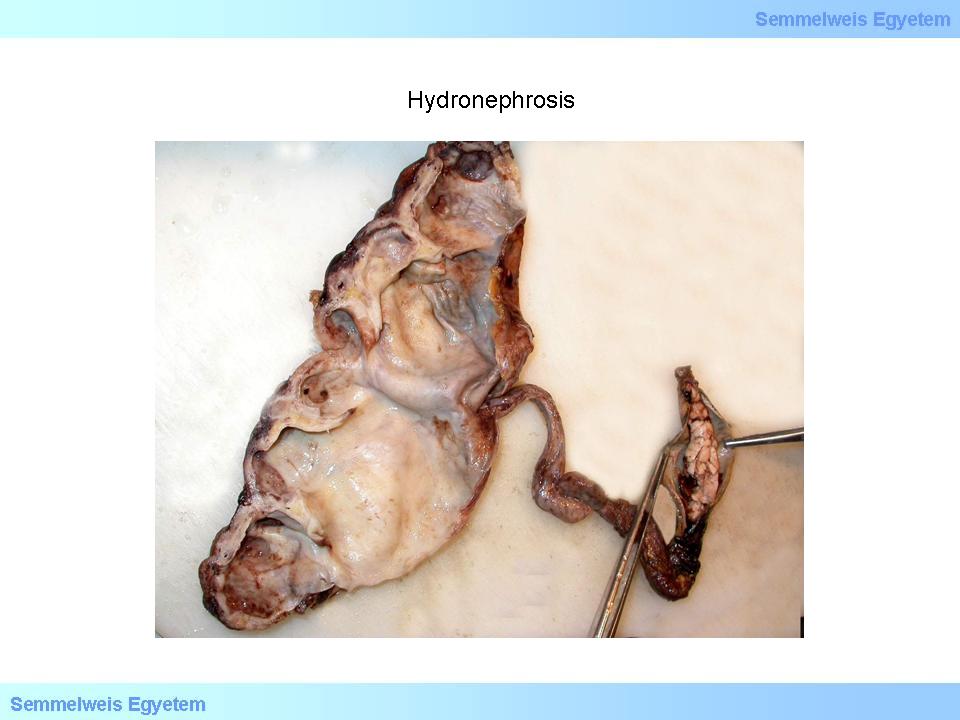
1st macropicture: Hydronephrosis. Transitional cell cancer in the ureter led to the development of a saccular kidney on the same side, with the almost complete atrophy of the renal parenchyma. (From the photo archive of the Semmelweis University 2nd Institute of Pathology – collected by Attila Kovács and Ildikó Szirtes).
|
|
 |
Causes of a bilateral hydronephrosis: trigone tumour, sclerosis of the inner bladder sphincter, prostatic hyperplasia, prostatic cancer (adenocarcinoma prostatae), cervical cancer, which spreads onto the urethra and trigone, urethral stricture, ’valve’ of the prostatic urethra, a so-called neurogenic bladder. Due to the urinal statis the tissue is stretched, which is compressing the small vessels and capillaries of the medullar and papillar parenchyma, therefore chronic ischaemia and secondary interstitial fibrosis and tubular atrophy develop. In case of a distal obstruction the muscles of the bladder overcome the obstruction with hypertrophy (trabecular hypertrophy), but later dilatation, diverticules caused by pea- or cherry-sized protrusions of the mucous membrane between the muscular fibers, a bilateral hydroureter and hydronephrosis occur.
|
 |
The distressed bladder muscle is not able to discharge the urine fully and a residuum of as much as 100 ml can remain within the bladder. The undischarged or stagnating urine will be infected with bacteria and first an acute, later a chronic urocystitis develop, leading to the occurrence of a pyelonephritis . Since the diverticules do not have their own muscular wall they are especially prone to retraining urine. The stagnating urine is a favoured place for bacterial propagation. Neonatal hydronephrosis is more common in boys. A valve-like mucous membrane in the prostatic part of the urethra and a stricture of the renal kidney-ureter junction (pyeloureteral stenosis) are the most important causative factors of neonatel hydronephrosis.
|
 |
Pyeloureteral stenosis can occur both in a uni- or bilater form. Unilateral stenoses are more common on the left side. Pyeloureteral stenosis in the adulthood is usually unilateral. It can be caused by congenital malformations manifesting later in life, or an aberrant branch of the renal artery supplying the kidney pole, which strangulates the pyeloureteral junction from the outside. In the third trimester of the pregnancy the foetus puts pressure on the maternal ureters. The developing hydronephrosis disappears after the delivery. A neurogenic bladder is a condition which develops if the function of the bladder is insufficient due to a disturbed innervation: e.g. in case of a laesion in the spinal motoneurons a functional dilation occurs; while in diabetic neuropathy a hypotonic, inert bladder develops, with a codeveloping hydoureter and hydronephrosis in both cases.
Morphologically the renal pelvis and calices are distended, the papillae are flattened, and the renal parenchyma is thinned, wasted because of the pressure. The atrophy occurs only in the papillae and in the medulla, but later it develops in the renal cortex as well. In end-stage hydronephrosis the renal parenchyma is thinner than 1 centimetre; the calices and the renal pelvis are markedly dilated in a sack-like manner and filled with stagnating urine. Histologically in the remaining papillary and cortical tissue atrophied renal tubuli and interstitial fibrosis are present. ’Pools’ consisting of Tamm-Horsfall glykoproteins, which entered the interstice through the ruptured tubuli can also be found, surrounded by lymphocytic-mononuclear infiltrations also present elsewhere. The cortical structure is fairly intact.
Glomeruli are open, proximal tubuli can be recognized, while distal tubular segments are dilated, many cross-sections are filled with eosinophilic substance. The renal capsule contains several wide lymphatic vessels. In case of a congenital pyeloureteral stenosis the muscular layer above the stenosis is thickened and the mucous membrane protrudes into the lumen in a valve-like manner. Histologically a circumscribed unorganization of the muscular layer’s muscle fibers can be observed, in which lengthwise fibers dominate.
|
 |
According to its clinical manifestation obstruction of the urinary tract is a frequently occuring condition, which can develop at any age. Its clinical features depend on the causative factor. Partial obstructions often lead to a hydroureter and to hydronephrosis without any symptoms. Unilateral hydronephrosis does not lead to declining kidney function, since the kidney on the other side substitutes the non-working kidney with hypertrophy. Bilateral hydronephrosis leads to decreased concentration capacity, azotaemia, renal hypertension and end-stage kidney failure. Main complications of distal obstructions of the urinary tract (e.g.: because of prostate hyperplasia) are: dilated hypertrophy of the bladder, diverticule of the bladder, urocystitis, hydroureter, vesicoureteral reflux, hydronephrosis, uni- or bilateral acute and chronic pyelonephritis.
I./2.3.2.: Urinary reflux and its complications (reflux-nephropathy)
|
 |
In its anatomical position the ureter pierces the bladder wall in an acute angle, so the final part of the ureter runs in the bladder wall obliquely from up to down, from the back to the front and from lateral to medial. This anatomical position makes it possible that urinary reflux does not occur - in spite of the almost always higher hydrostatic pressure in the bladder – neither during passing urine (miction) nor between urinations, at rest. During these resting stages the anatomical buildup of the ureter orifices is sufficient in its own to passively avoid urinary reflux: the higher pressure in the bladder compresses and closes this final part of the ureter, which has a constantly thinning wall (looking from the inside of the bladder).
Along this closing, which is strengthened by natural valve-like mucous faults, the peristaltic moves of the ureter forward a few centimeter long ’urine roll’ to the bladder. Between these peristaltic waves the urine does not flow back from the bladder not even with a relaxed ureteral wall. During urination the contracting bladder muscle thightens and closes the lowest, intramural part of the ureter with its active muscle contraction (without having a distinct muscle ring (sphincter)), helping to prevent the urinary reflux this way as well.
If – due to a developmental anomaly – the ureter enters the bladder wall less acutely, in some patients even squarely, then the intramural ureter part is short (sometimes the longitudinal muscle fibers of the ureter do not even develop). Therefore, the above described closing mechanisms of the ureter do not work properly, and the urine flows back to the ureter (vesicoureteral reflux), or even to the renal pelvis, to the calices and in unfortunate cases even into the kidney (intrarenal reflux). In case of an intrarenal reflux the urine flows back to the kidney mainly through the papillae of the upper and lower pole. Since the papillary surface is concave, the papillary ducts opening on them close less properly. This explains not only why the reflux is more severe on the kidney poles, but also why the resulting renal inflammation, chronic pyelonephritis affect the renal poles more often and in a more severe way.
|
 |
If the vesicoureteral reflux is of high pressure the renal pelvis and calices enlarge, and the backflowing urine results in the inflammation and scarification of the lower and upper pole (reflux nephropathy). The vesicoureteral reflux and reflux nephropathy can be both uni- and bilateral. The degree of the reflux can be increased by an adjoining lower urinary tract obstruction. If the urine in the bladder is overinfected by bacteria, then the refluxing urine causes an upper urinary infection and (as a part of it) an acute, and later a chronic renal inflammation develop. If the upper urinary infection reoccurs, an extensive scarrification develops. Consequently, the kidney gets smaller (renal atrophy), the border of its upper and lower poles becomes irregular, markedly retracted, and small scarifications appear in its middle third as well.
|
 |
On the microscopic surface the scars are present above the flattened papillae having concave apexes. Here the cortical tissue is sometimes thinner than even 0.5 centimetres. The enlarged calices and renal pelvis extend directly to the thinned cortex. Histologically chronic tubulointerstitial damage with distinct borders of both the cortical and medullar parenchyma can be observed: interstitial fibrosis, tubular atrophy, lymphocytic infiltration in the interstice and focal glomerular scarification are present. Several atrophied tubuli aluminal, while others are rather dilated; their epithelium cover is flattened, with eosinophil cylinders in their lumen. Reflux nephropathy rarely occurs on its own; it is almost always accompanied by ascending pyelonephritic lesions.
Because of this, vesico-ureteral reflux is usually discovered during assessments of recurring infections of the upper urinary tract. Infectious episodes are unavoidable; progressing focal renal scarring leads to renal hypertension and secondary glomerular scarring and proteinuria. In case of a bilateral process a final stage kidney failure (end-stage kidney) develops. Hypertensive disorders in childhood and adolescence are most often caused by reflux nephropathy.
I./2.3.2.1.: Acute pyelonephritis (acute bacterial tubulointerstitial nephritis)
|
 |
Bacteria settle and proliferate in the renal insterstitium, causing an acute, often purulent inflammation. At the same time, almost inseperatedly from this process, an inflammation of the calices and the renal pelvis occur as well (pyelonephritis). The inflammation of the kidney is caused by an ascendent urinary infection in most cases (reflux nephropathy is a severe risk factor); while pathogens reach the kidney through the blood flow in a small proportion of cases (especially in septic disorders, e.g. during the so-called embolic focal nephritis of acute/subacute endocarditis).
Pyelonephritis can be uni- or bilateral. In case of an ascending infection first an acute urocystitis develops and then the pathogens reach the renal pelvis and finally the kidney through the ureter. Animal studies suggest that pathogens adherent to the tubular epidermal cells are being incorporated by the epidermal cells through endocytosis. Pathogens multiply in the epidermal cells, and they destroy the cells with their endotoxines, finally reaching the interstice. Ascending infections can occur both in case of normal anatomical structures and in case of malformations of the urinary tract. In the latter case also the cleaning-diluting-flushing function responsible for the sterility of the urinary tract is damaged.
|
 |
Acute pyelonephritis developing along intact anatomical structures occurs most often in women between 18-40 years with an active sexual life. The pathogen is of faecal origin, in most cases the uropathogen E. coli, which is able to attach and proliferate on the uroepithel due to its special characteristics, such as the ability to bind to fimbriae, haemolysin, aerobactin, uroepithelial receptors.
Pyelonephritis occurring as a complication of nephrological or functional abnormalities of the urinary tract develops in all ages. It is most common among newborn and infants and among the elderly. Important risk factors include pregnancy, diabetes and immunosuppressed states. If a tube is placed to the bladder to drain urine (catheterization) or transurethral procedures (scoping of the urinary bladder, of the ureter or the renal kidney, or a transurethral resection – TUR) are performed so-called hospital bacterial strains can settle and proliferate in the urinary tract (nosocomial infection).
Nosocomial infections caused by catheters of the urinary bladder make up to 40% of all hospital infections! The pathogen of pyelonephritis is E. coli in most cases, but Proteus mirabilis, Serratia-, Enterococcus-, Pseudomonas, Klebsiella, Staphylococcus aureus, and Candida-infections are also common. These pathogens do not have uropathogenic features. Some of them are resistant to antibiotics.
I./2.3.2.2.: Acute apostematous pyelonephritis
|
 |
The kidney is slightly enlarged, with numerous, yellow-white, nodules of 1-3 millimetres flatly emerging on its surface (microabscess) (2nd macropicture). On the cut surface confluent nodules are present both in the cortical and medullar parenchyma. In the renal pyramides fan-shaped or parallel yellow, thin stripes are running to the papillae can be observed (the formulae are equivalent to renal tubuli filled with neurophils. The mucous membrane of the calices and the renal kidney is bright red. Histologically smaller-bigger acute abscesses can be observed, with an oedemic interstice infiltrated with neutrophils and macrophages. Neutrophils clink to the basal membrane of the tubuli and they infiltrate the tubular wall. Equivalent to the fan-like stripes cylinders with purulent cells are present long within the tubuli.
|

Look at the picture and analyze it!
|
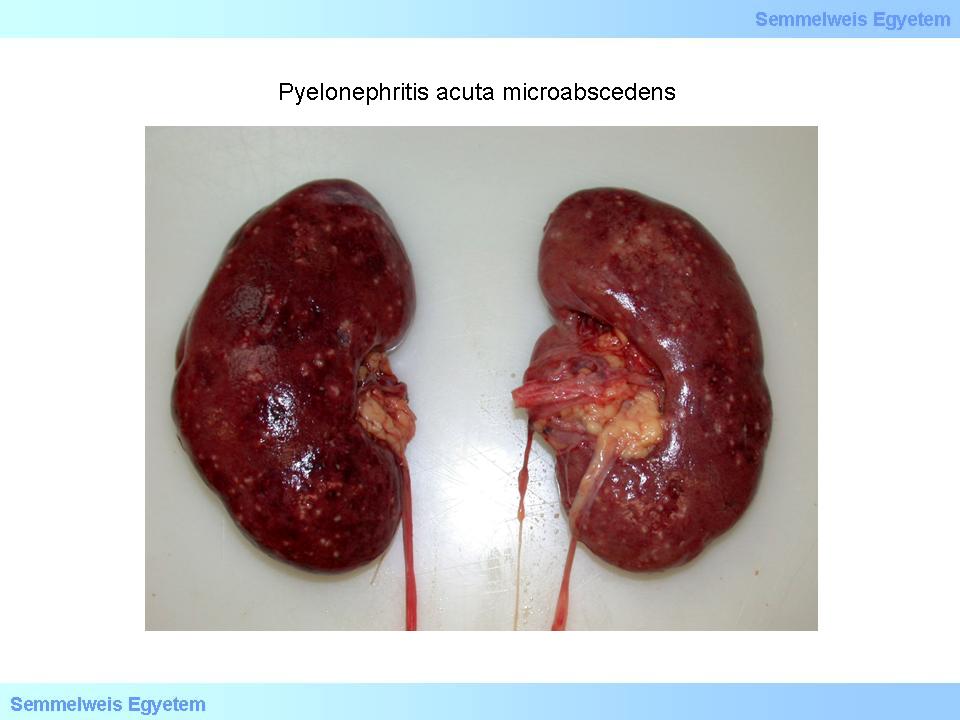
2nd macropicture: Acute pyelonephritis microabscedens. On the surface of both kidneys several pointlike absceding foci are present. (From the photo archive of the Semmelweis University 2nd Institute of Pathology – collected by Attila Kovács and Ildikó Szirtes).
|
In case of an ascending urinary infection the interstitial leukocytic infiltration usually does not affect the glomeruli (1st micropicture). If bacterial colonies and suppuration can be seen in the glomerulal capillaries, the diagnosis of a pyelonephritis of haematogenous origin has to be considered. Supporation heals with scarification. Mild cases cured successfully with antibiotics on time can heal completely, without marks. On the contrary, in severe cases papillary necrosis can occur as a complication of urinary obstruction, diabetes or use of analgetics. If the obstruction is complete a purulent sacculent kidney (pyonephros) develops. Small, confluent abscesses can sometimes compose centimeter-long abscesses: intrarenal abscesses (renal carbuncules) develop.
|

Look at the picture and analyze it!
|
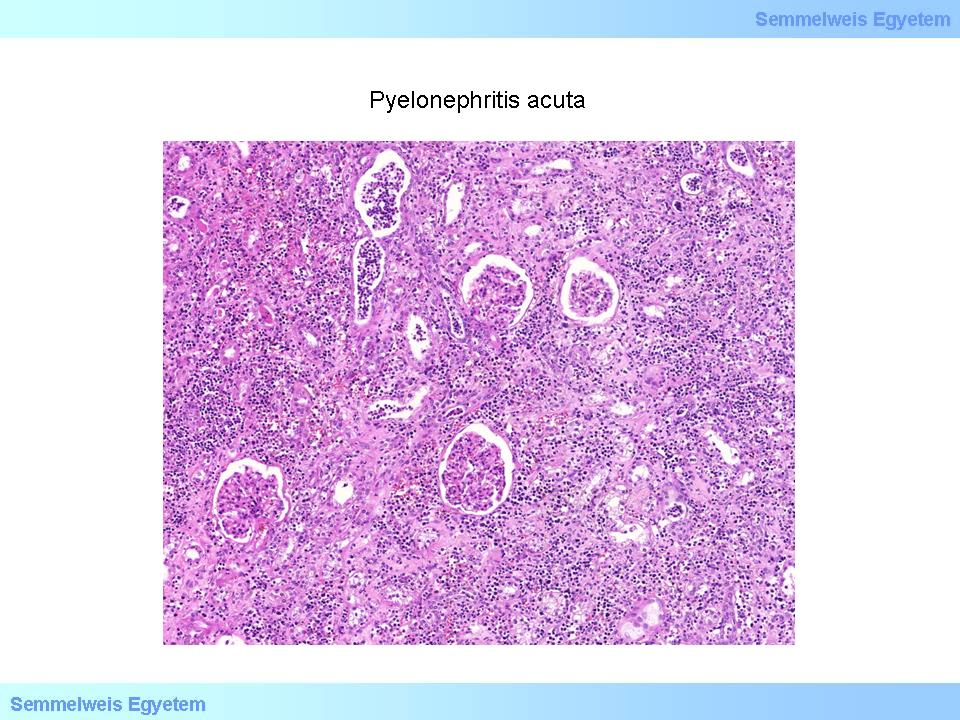
1st micropicture: Acute pyelonephritis. In the renal parenchyma an infiltration of mixed inflammatory cells of marked degree is present. In the tubular lumens a great number of granulocytes can be observed. Glomeruli are usually not involved in the process. (From the photo archive of the Semmelweis University 2nd Institute of Pathology – collected by Attila Kovács and Ildikó Szirtes).
|
A perirenal abscess develops if the suppuration breaks through the fibrous capsule (capsula fibrosa renis). Pus cumulates in the adipose tissue and can even spread till the Gerota’s fascia. The diagnosis of an acute pyelonephritis can be set unambiguously up by the symptoms of suddenly developing high fever, shivers, pain and sensitivity in the kidney area, costovertebral tenderness, leukocytosis, symptoms of passing infected urine (frequent and commanding urination stimulus, burning urination), pyuria and significant bacteriuria (105 bacteria/ml urine). Pyelonephritis developing in case of normal anatomical structures is of good prognosis if the pathogen is sensitive to antibiotics. Pyelonephritis developing as a result of abnormal anatomical structures can have different outcomes; mild, moderate, severe and lethal cases can occur as well. The causative factor, the inflammatory process itself and the complications of pyelonephritis all have a great influence on the prognosis. Severe malaise, hypotension and impaired consciousness all refer to urosepsis. Classic symptoms of acute pyelonephritis are missing in infancy and small children. Recurrence is not rare because of drug-resistance and persistant urinary obstructions.
I./2.3.2.3.: Acute emphysematous pyelonephritis
|
 |
It is caused by gas-producing E. coli infections in diabetic patients. Gas-containing cavities develop in the renal cavity, parenchyma and retroperitoneal tissue. Abscesses and an extensive necrosis of the parenchyma can be observed. The disease is fast in its course and often lethal. A nephrectomy, opening and evacuating the area can be life-saving.
I./2.3.2.4.: Chronic pyelonephritis
|
 |
Focal scarring which develops because of the chronic damage of the interstitice and tubuli of the cortical and medullar tissue. Papillae under the scar are flattened and the calix is wide. The damage is caused by asymptomatic, latent bacterial renal infections associated with reflux and/or obstruction. Chronic pyelonephritis can be uni- or bilateral. The kidney can be atrophied – even as little as 50 grams -, its surface - especially above the poles - is made roughly uneven by extensive, irregular, map-like retractions. On the microscopic surface the scars reach the papillae, which are flat and the joining calix is wide and deformed with a thickened mucous membrane. In case of a reflux the scars are more marked in the lower and upper poles.
For a differential diagnosis it is important to mention that the circulatory-based (nephrosclerotic), infarcted scars are wedge-shaped and do not always reach the medullar parenchyma and are accompanied by intact, not widened calices below them. The inflammatory-based (pyelonephrotic) scars and the surface retractions caused by them are however irregular and map-like with an extensive area. The area involved does not confine only to the supply area of a single vascular branch, it extends to the whole parenchyma. The adherent calices are wide.
Histologically focal tubulointerstital damage (with interstital fibrosis, atrophic tubuli and with focal mononuclear and lymphocytic infiltration of the interstice) is present in the whole thickness of the renal parenchyma. Because of the tubular damage the glomeruli get closer to each other and a circular fibrosis can be seen around the Bowman’s capsule. Most of the glomeruli are atubular. The remaining atrophic tubuli are wide and stagnant. Since they are filled with eosinophilic cylinders, the picture is reminiscent of thyroid tissue (renal thyreoidisation) (2nd micropicture). In the inflammatory infiltrate lymphatic follicles can develop, especially periarterially. If a latent bacterial infection is still present in the parenchyma, then in the granulocytic cylinders are present in the papillary and cortical tubuli, while in the insterstice neutrophils can be found sparsely.
|

Look at the picture and analyze it!
|
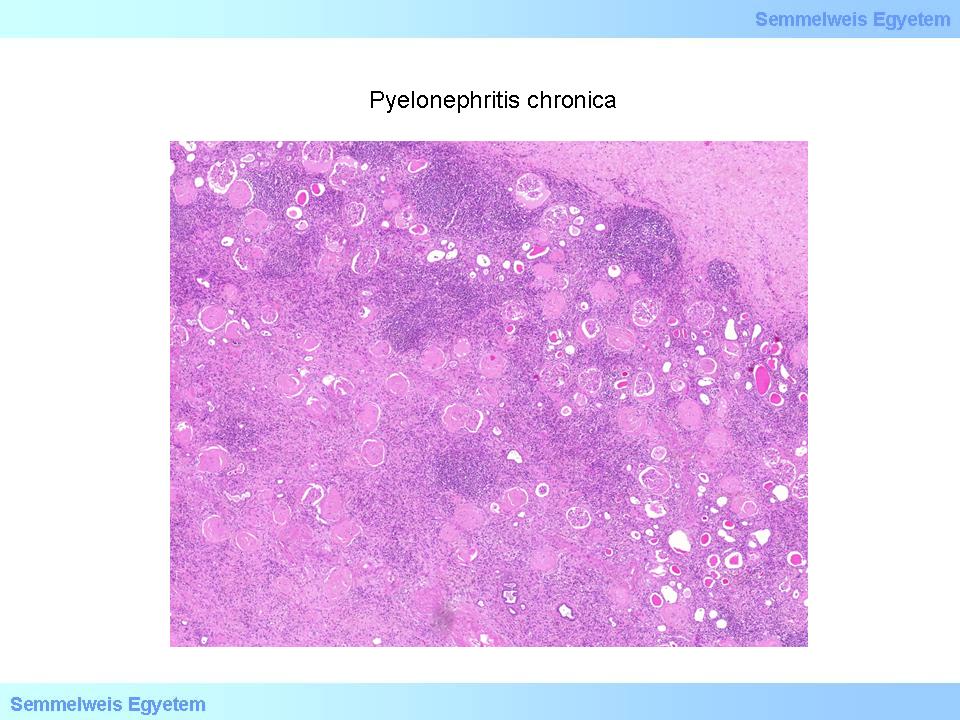
2nd micropicture: Chronic pyelonephritis. In the renal parenchyma tubular atrophy and consequent fibrosis, a marked chronic inflammatory cell infiltration can be seen. Glomeruli are hyalinized, the majority of them entirely, while a few glomeruli only partially. On the right side of the picture the group of atrophied tubuli filled with eosinofilic substance recalls thyroid tissue. (From the photo archive of the Semmelweis University 2nd Institute of Pathology – collected by Attila Kovács and Ildikó Szirtes).
|
On arteries/arteriolae passing through the scars intimal fibroelastosis occurs. Both under the urothelium of the calices and the renal kidney in a small stripe macrophages, lymphophages, lymphatic follicules and sparsely neurophils can be observed. Inflammatory cells spread onto the urothelium. In clinical practice chronic pyelonephritis is a common disorder of the kidney. In its unilateral form renal function can remain within the physiolocial range even with severe atrophy due to the compensation effect of the other kidney (compensatory or vicarious renal hypertrophy), however, unilateral scarring leads to renal hypertension. Its bilateral form causes a slowly progrediating azotemia, renal hypertension, hyperfiltrative glomerulus damage and a consequent proteinuria. In some patients an end-stage kidney develops. In Hungary more than 10% of patiens undergoing heamodialysis suffer from chronic pyelonephritis as a primary disorder.
I./2.3.2.5.: Pyelonephritis xanthogranulomatosa
|
 |
In certain cases, mainly in middle-aged women with diabetes and kidney stones
Escherichia coli, Proteus mirabilis or Staphylococcus aureus infections are associated with a long, unilateral purulent-granolumatous pyelonephritis containing macrophages with foamy cytoplasms develops.The occurring condition destroys the medulla. Granulomatous reactions are caused by prolonged suppuration and tissue destruction and by continuous bacterial presence. Electronmicroscopically it can be observed that the foamy cells, which are dominating the inflammation are present en masse. In the beginning the foamy cells contain bacteria continuously, which are later joined by several phagolysosomas and some amorph material as well. The kidney is enlarged. The renal pelvis and the calices are thickened and broad. They can contain coral-like (thorny) stones and tissue debris.
The papillary apexes are demolished. Medulla has been replaced by abscesses and yellow, at parts bloodshot areas. In the cortex rough scars have developed. The fibrous capsule is thickened, interlocking with the perirenal fat tissue.
Histologically the yellow tissue foci consist mainly of macrophages with foamy plasma, smaller macrophages with PAS-positive cytoplasma, lymphocytes, neurophil granulocytes and plasma cells. Fibroblasts and multinodular giant cells can be present as well (3rd micropicture). Inflammatory cells can form granulomas. Chronic suppurative inflammation is present in the mucous membrane of the calices and the renal pelvis. In the cortex a secondary parenchymal scarring occurs. It is a rare phenomenon, which can mimic renal cell carcinoma radiomorphologically, therefore leading to an unnecessary kidney removal. In its excessive form the kidney can be unable to function. In these cases – since the body is unable to overtake the bacterial mass present – even nephrectomy can be discussed as a final solution.
|

Please take a look at the picture!
|
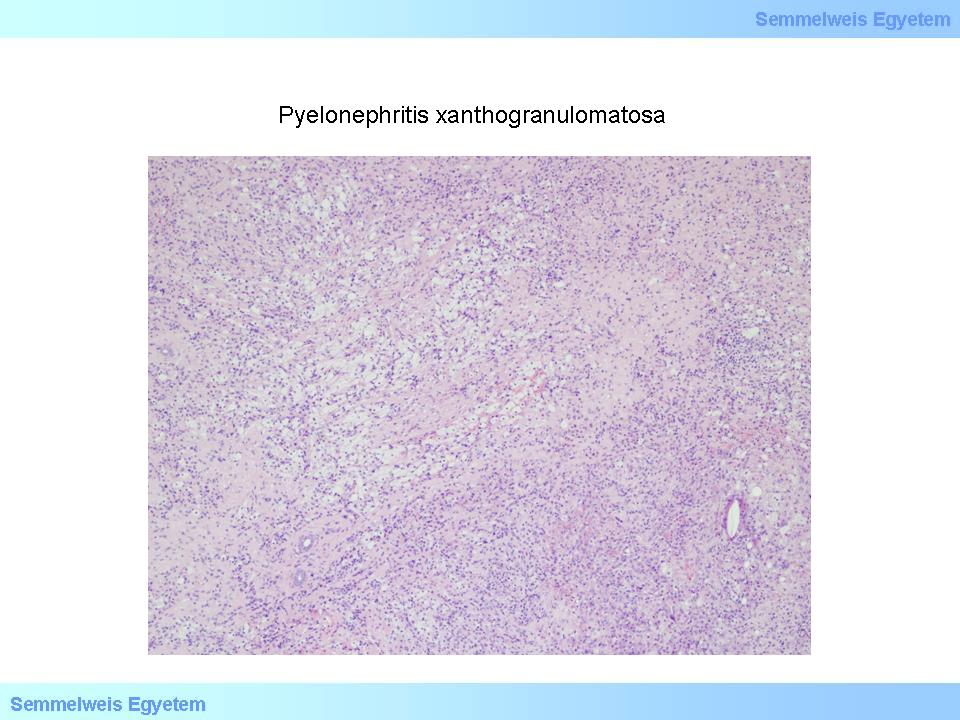
3rd micropicture: Pyelonephritis xanthogranulomatosa. Neoplastic process could not be verified in the area clinically suspected. Lateral to a bloodshed cyst (not present on the photo) histologically an explicit xantogranulomatous inflammation with chronic infiltration of inflammatory cells was present. A few atrophied tubular cross-sections and foreign body reactions to dissolved cholesterol crystals can be observed in the area as well. (From the photo archive of the Semmelweis University 2nd Institute of Pathology – collected by Attila Kovács and Ildikó Szirtes).
|
I./2.3.2.6.: End-stage kidney and renal failure (renal insufficiency)
|
 |
End-stage kidney is the final state of chronic kidney disorders of all origins. In Hungary end-stage kidney develops mainly as a result of primary glomerular disorders. Other conditions include diabetic nephropathy, lupus nephritis, chronic interstitial nephritis and polycystic kidney in adults. Patiens involved are suffering from chronic uraemia. Uraemic toxins cause an acute inflammation on serous membranes (typically with fibrinous exudate, see the sterile fibrinous pericarditis in uraemic patients and in the gastrointestinal tract while in the brain uraemic encephalopathy occurs. If it is not possible to replace kidney function (dialysis) encephalopathy results in a uraemic coma, and the patient dies.
The atrophied kidneys cause a hypertension of renal origin; they do not produce erythropoetin and the vitamin D metabolism is also damaged. Macromorphologically the kidneys are markedly atrophied, weighing less than 50 grams each. On the scarry cut surface the cortical and medullar parenchyma can not be differentiated. Severel cysts with a serouos content are present in the whole parenchyma. Histologically in the arteries obliterative intimal fibrosis, sclerotic glomeruli, interstitial fibrosis with developing scarring can be observed; in the cicatricial ground tissue atrophied tubular remains are present far from each other. Most of the fibrotic glomeruli can not even be recognized with special staining.
In the heart renal hypertension causes hypertrophy in the left ventricule, while uraemic toxins cause cardiomyopathy and a sterile fibrinous pericarditis. In the brain in a uraemic coma a severe oedema develops; hypertension can lead to a stroke. In peripheric nerves a uraemic neuropathy occurs, which is primarily characterized by the degeneration of axons and the depletion of nerve fibers, secondarily by a segmental demyelinisation. Clinically a disturbed sensation occurs in the lower extremities (impaired deep sensation and sensation of vibration). Some men complain of erectile dysfunction. In the lungs alveolar odema rich in proteins occurs with the development of hyaline membranes (uraemic pneumonitis). On the pleura a sterile fibrinous inflammation develops. The development of uraemic pneumonitis has been successfully lowered by accurately performed dialysis. In the gastrointestinal tract an acute mucous oesophagitis and gastritis and mucous or pseudomembranous colitis can occur. In the pancreas an acute necrotizing haemorrhagic pancreatitis might develop.
|
 |
The parathyroid gland becomes hyperplasic mainly because of hypocalcaemia, the synthesis of parathormone increases, clinically hyperparathyreosis develops. In the bones the osteoclast activation caused by the hyperparathyreosis thins the bone trabecules, which are replaced with fibrovascular tissue rich in multinuclear giant cells. In the tissue haemorrhages, hemosid deposits and cystic degenerations are present. Clinically bone pain, sometimes pathological breaks develop. The calcium dissolved from the bones sediments in the soft tissues, arteries and in the places of H+-discretion (in the lung, stomach and - in case of a remaining acidifying capacity - in the kidneys as well) during the process of pathological calcification. The calcification of arteries, the uraemic toxins and the hypertension make the atherosclerosis severely worse.
Tendons and cartilages are affected by amoloidosis, which develops in patients kept alive with 6-8 years of dialysis causing joint deformities and/or carpal tunnel syndrome in these localizations. The amyloid protein in these patients is the ß-2-microglobulin. The microglobulin fragment freely filtrates on the glomerular basal membrane (GBM) of the healthy kidney, but not on the semi-permanent membrane of the dialysis machine. In the bone marrow the red blood cell production decreases because of the erythropoietin deficit, therefore the patients suffer from chronic anaemia (haemoglobin concentration < 11 g/dl, haematokrit < 33%). In the skin uraemic paleness, itching (pruritus) and a prolonged wound healing occur. Uraemia disturbs the immune regulation, so infections are frequent (e.g.: bacterial pneumonia, viral respiratory infections).
Clinically the patiens in the state of an end-stage renal failure can be kept alive with treatments aiming to substitute for renal function - haemodialysis, peritonealis dialysis -, or with a renal transplant. On ultrasound imaging small, contracted kidneys can be observed. A significant part of patients undergoing renal function substitution for years die because of cardiovascular disorders (myocardial infarction, heart failure, ischaemic stroke, haemorrhagic stroke, or infections. A typical complication of peritoneal dialysis is acute purulent peritonitis occurring because of bacterial overinfection. If the complication is recognized on time, a forceful antibiotic treatment can save the patient’s life.
I./2.3.2.7.: Hypertensive disorder (high blood pressure, hypertension)
Vide chapter ’Myocardial infarction and its consequences’.
I./2.3.3.: Divided kidney (kidney divisum), double renal pelvis and ureter (pyelon and ureter duplex)
|
 |
It is the most common developmental anomaly of the urinary tract. Supernuminary kidneys (i.e. two, distinct kidneys on the same side) are extremely rare, while its abortive form, the divided kidney (kidney divisum) is more common: the kidney is slightly enlarged and in its middle third it is divided into two equal parts by a parenchymal septum running from the convexity to the renal hilum. Such a kidney consists usually of two independent renal pelvises surrounded by their own peripelvic fat tissue (pyelon duplex). From each pyelons opens a separate ureter. If the ureters remain separated in their whole run and they open into the bladder with a double ostia then they are called double ureters (ureter duplex). If the two ureters join and open into the bladder with one, joint confluence the condition is called ureter fissus.
I./2.3.4. Ureterocele and ureter prolapse
Ureterocele is a condition where the ureter balloons at its opening into the bladder. In the background of the condition a congenital stricture of the ureteral opening is present, so the urine passes from the ureter with difficulty and increased pressure, which protrudes the mucous membrane. This protrusion of the mucous membrane can even fill half of the urinary bladder. In ureteroceles kidney stones can develop. With time the lesion causes the widening of the ureter and the renal pelvis (hydroureter, hydronephros).
|

Please take a look at the picture!
|
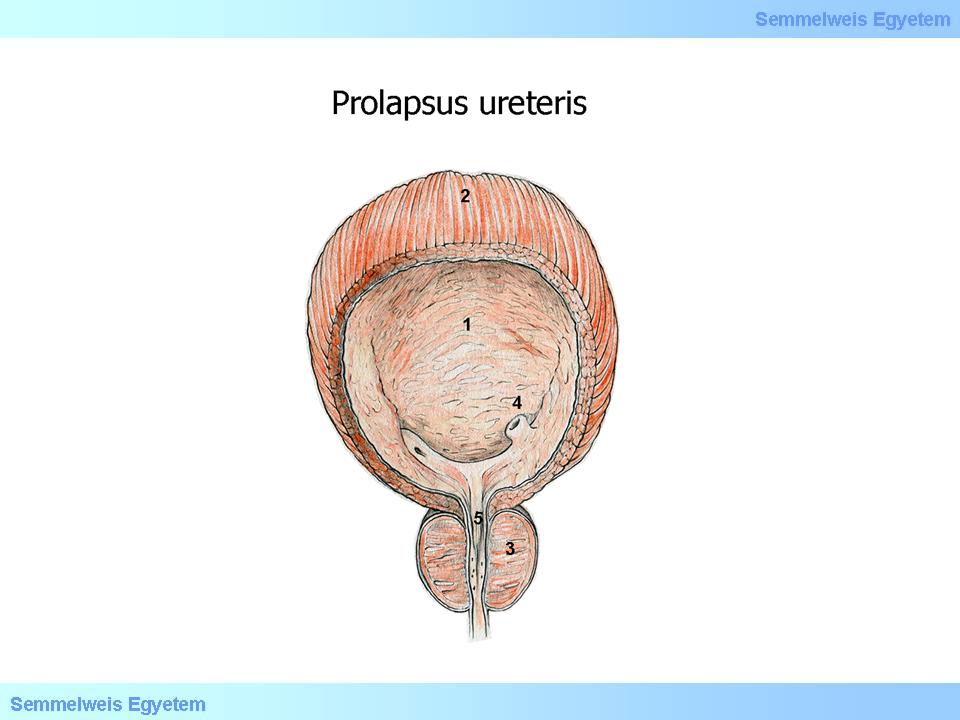
Illustration 1: Prolapsus ureteris (Kiss Balázs): (1) Vesica urinaria; (2) Musculus detrusor uretrae; (3) Prostata; (4) Ureter prolapsus; (5) Uretra
|
|
 |
A malformation very similar to the ureterocele is the ureteral prolapse, which is the shared protrusion of the bladder wall and the ureteral wall into the urinary bladder around the orifice. The protrusion here does not only consist of the mucous membrane but of the layers of the bladder and ureter walls as well. It is a rare developmental anomaly which is often associated with other developmental anomalies of the urinary tract, especially with a double ureter (ureter duplex) and megaloureter. Both conditions can be diagnosed with excretory urography.
I./2.3.5. Hydrourterer, megaloureter
Hydroureter is an acquired dilation of the ureter, while megaloureter is the congenital from of ureteral dilation. The latter one, just like the intestinal Hirschsprung’s disease also develops because of a congenital neuromuscular dysplasiaof a certain part of the ureter (the prevesical/distal part). The missing peristaltic movements caused by the dilation serve as a functional obstruction, so the transmission of the urine is deficient, which leads to an extreme dilation of the whole proximal part of the ureter.
The stagnation is augmented since the run of the dilated ureter becomes crooked with buddings and breaches. The dilation does not lead to the thinning of the ureteral wall since its muscle transforms into connective tissue and the excessive tissue compensates the thinning caused by the dilation. Urinal stasis often leads to ascending urinary infections, and infections with a gradually developing hydronephrosis lead to further parenchymal distruction. Although the disorder can remain asymptomatic for years, untreatedly it leads to the complete failure of the kidney on the same side.
I./2.3.6. Calculi (nephrolithiasis, ureterolithiasis, vesicolithiasis, urolithiasis)
|
 |
Three factors play an important role in its development: (i) salts present in the urine, which tend to crystallize, (ii) a ’nucleus’ starting the crystallization process, and (iii) the abscence of substances preventing crystallization. In case of a calculus the urine is oversaturated with ions of salts inducing calcification, while diluted and rich diuresis normalizes the oversaturation. The microscopic crystallization foci (nidus) initiating the crystallization process can either consist or tubular epithelium cells, cell fragments, inflammated exudate fragments or cleared tubular cylinders or uric acid crystals as well. The ’nucleus’ adheres to the urothelium of the renal calix and the oversaturated solution’s salts precipitate onto its surface. If the calculus grows big enough it can even fill out the shape of the renal pelvis like a casting (so-called coral stone or thorny stone). This can result in dilated calices without a kidney stone attack, and parenchymal damage/atrophy in the involved parts.
|

Please take a look at the picture!
|
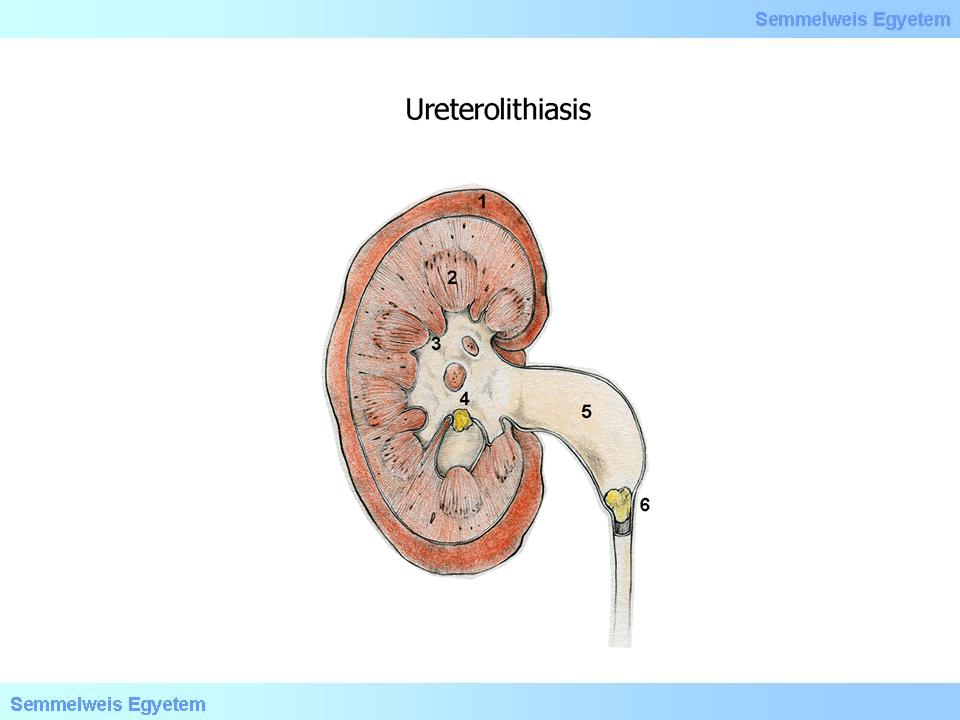
Illustration 1: Ureterolithiasis (Kiss Balázs): (1)Cortex renalis; (2) Pyramis renalis; (3) Papilla renalis; (4) Vesekő a pyelonban; (5) Urether tagulat; (6) Hugyúti obstrukciót okozó vesekő.
|
If the developing stone remains small, urine flow can wash it to the ureteral orifice or even more deeply into the ureter, where it can wedge into the lumen. The inclusion can be worsened by a reflexive spasm triggered by the ureter damage caused by the stone’s uneven surface, and the urine becomes obstructed. Urine obstruction is associated with cramps (kidney stone attack, ’kidney spasm’, griping). This is why the saying ’small stone small problem, large stone big problem’ is true. Acidic macroproteins (nephrocalcin, uropontin, Tamm-Horsfall’s protein) prevent calcification. The citrate content of the urine is another preventing factor, since citrate increases the solubility of calcium oxalate. The urinal pH is also an important factor. ’Alcalic’ values above pH=6.5 favour the oversaturation of calcium phosphate.
65% of the stones consist of calcium-oxalate or calcium-oxalate and calcium-phosphate. The stones are hard, black-brown, with a size of 1-2 centimetres and sharp borders. On the X-ray the kidney stones display as shadows. The development of struvite stones is potentiated by kidney infections (struvite: an ammonium-magnesium-phosphate crystal containing water (NH4)MgPO4+6H2O], which is formed easily in human and animal urine if the urine is infected with ammonium-producing bacteria). Struvite stones are grey-yellow and relatively soft, filling the renal kidney similar to deer horns. They are also present as shadows on X-ray films. Uric acid stones (15%) are white or orange, they can fill the renal pelvis and they do not appear on an X-ray.
Pain caused by stones reaching the ureter and moving down is one of the complications of kidney stones, just like micro- and sometimes macroscopic haematuria caused by the excoriation of the urothelium. Partial or recurrent ureter occlusion leads to hydronephrosis, and to pyelonephritis, in case of an infection. In the clinical practice renal stones occur mainly among the middle-aged, but stones can also develop in childhood. It is a frequent disorder and can occur both uni- or bilaterally. A kidney stone attack consists of intense lumbocostal, sometimes upper abdominal cramps (colic pain), haematuria and an urgent, painful urination stimulus. The pain radiates to the groin, to the labia majora or to the testicles with a growing intensity. An ultrasound confirms an acute unilateral dilatation of the pyelon and the calices and the stone can usually be detected. The pain stops when the stone reaches the bladder.
|
|