| |
II./4.6.: Therapy
It is generally accepted that only symptomatic lesions should be treated. In case of myoma, diagnosed in asymptomatic patients, treatment is not necessary, but regular monitoring is required. The selection of the appropriate therapy is determined according to the patient's age, childbearing intention, the severity of symptoms, the size and location of the myoma.
Medication.
|
 |
The goal of using different hormone formulations with different target points is to reduce bleeding and the size of the myoma. The most commonly used products are: birth control pills, GnRh agonists/antagonists, gestagenes, progesterone receptor antagonists (mifepriston) and selective progesterone receptor modulator (SPRM) formulas (asoprisnil). Recently, treatment with ulipristal acetate seems to be the most promising: during a 3 months treatment it significantly reduces the size of the uterus with the myoma and also the complaints. Its common characteristic is that the effect is limited to the duration of the treatment, it does not give definitive treatment and during the use a number of side effects are to be expected. In the treatment of hypermenorrhoea associated to myoma, the use of a levonorgestrel-releasing intrauterine device (IUD) is the most common method. Widespread use in some countries significantly reduced the number of hysterectomies performed because of excessive bleeding.
Surgical treatment.
Hysterectomy. Recommended in case of a symptomatic, large myoma which is growing and if the patient is older than 35-40 years and does not want to be pregnant any more. Fibromas are the most common indication for hysterectomies (32%), the second in line is abnormal uterine bleeding (17%). Intervention is the definitive treatment of the disease, as it is 100% effective and the possibility of recurrence is not to be expected. The most common form is abdominal hysterectomy (60%). The advantage of this is that during open surgery even the extreme size uterine myoma (length above the belly button) is relatively easy to remove quickly. The disadvantages are the larger incision and longer recovery (4-6 weeks).
|
 |
In case of medium and small size uterine myoma, vaginal hysterectomy is the method of choice, if all operating conditions are fulfilled. The advantage of vaginal hysterectomy is that there is no abdominal incision, hospital stay and recovery period are shorter (4 weeks). Abdominal surgery in the history, no prior delivery, and any other co-indication for surgery (e.g. ovarian cyst) may constitute a contraindication for vaginal solution. In these cases, laparoscopic hysterectomy is recommended. The advantages of laparoscopic surgery are better visualization, reduced surgical damage, short hospital stay (1-2 days) and rapid recovery (2-3 weeks). The disadvantage of laparoscopic surgery is the longer operative time.
In case of vaginal and laparoscopic hysterectomy, in 3-4% of the cases conversion to laparotomy is necessary due to intraoperative complications or technical problems. The major complications related to hysterectomy could be an injury to the urinary bladder, ureter and the intestines, their frequency varies between 1-3%, depending on the used method. Of long term complications - even if sparing the ovarian - earlier menopausal symptoms (3-4 years), more frequent urinary incontinence (hazard ratio 2.4) and vaginal prolapse (cumulative incidence of 0.5% -2%) are to be highlighted.
Myomectomy.
In case of intention to having children, the primary goal of therapy is to remove all myoma nodules and maintain healthy tissues while preserving fertility. Myomectomy can be performed with laparotomy, laparoscopy, hysteroscopy or by vaginal surgery. With laparotomy all of the nodules can be removed regardless of size and number. Laparoscopy is recommended if the sizes of the nodules are between 5-10 cm and it is not multiplex, since multiple wound care (sutura) and dissection of the nodules (morcellatio) significantly increases the duration of surgery.
Laparoscopic myomectomy is favorable when comparing the complications, with laparotomy, but difference cannot be detected in the fertility results for subsequent periods. The optimum technique for removing submucosal nodules (5 cm) is hysteroscopic myomectomy. The advantage is the short nursing care (1-2 days) and rapid recovery (1-2 weeks); disadvantage is the risk of uterine perforation and fluid overload. Cervical nodules and gelatinized submucosal nodules nascent through the cervical canal can be removed vaginally. For the latter intervention blood transfusion preparedness is required because of the risk of heavy bleeding.
|
 |
Compared to hysterectomy, major surgical blood loss is more common during myomectomy, but urinary bladder, ureter and bowel injury rarely occurs. In the early postoperative period, wound infection frequency is about 5%, the number of febrile complications can reach 30%, while transfusion is needed in 5-20% of the cases. Among the late complications, adhesion formation must be pointed out that may occur with over 50% frequency after myomectomy. The formed adhesions may adversely affect the subsequent fertility when the ovaries and fallopian tubes are also affected.
Investigations with long-term follow-up show that 5 years after myomectomy in nearly 50% of the patients recurrence occurred and in 10-25% of the cases a second surgery was required. Larger uterine size and multiple nature of the lesion experienced during myomectomy increases the risk of recurrence (in case of multiple nodules, the relative risk of relapse was 2.4, compared with those who had only one nodule).
Embolization of the uterine artery (Uterine Artery Embolization-UAE).
This minimally invasive treatment method of uterus myomatosus gravis can be recommended for those who reject the traditional surgical treatment options. The intervention is performed by interventional radiologist after gynecological examination and consultation. During the procedure via femoral or radial artery, under X-ray guidance a catheter is positioned to both uterine arteries and embolization of the ascending branches is performed either with tris-acryl gelatin micro-particles or polyvinyl-alcohol (PVA) particle. As the uterine arteries are responsible of nearly 90% of the blood supply of the myoma, their obliteration may cause the cessation of blood supply to the tumor. As a result of necrosis the volume of the tumor decreases by 30-70%.
|

Please take a look at the picture!
|
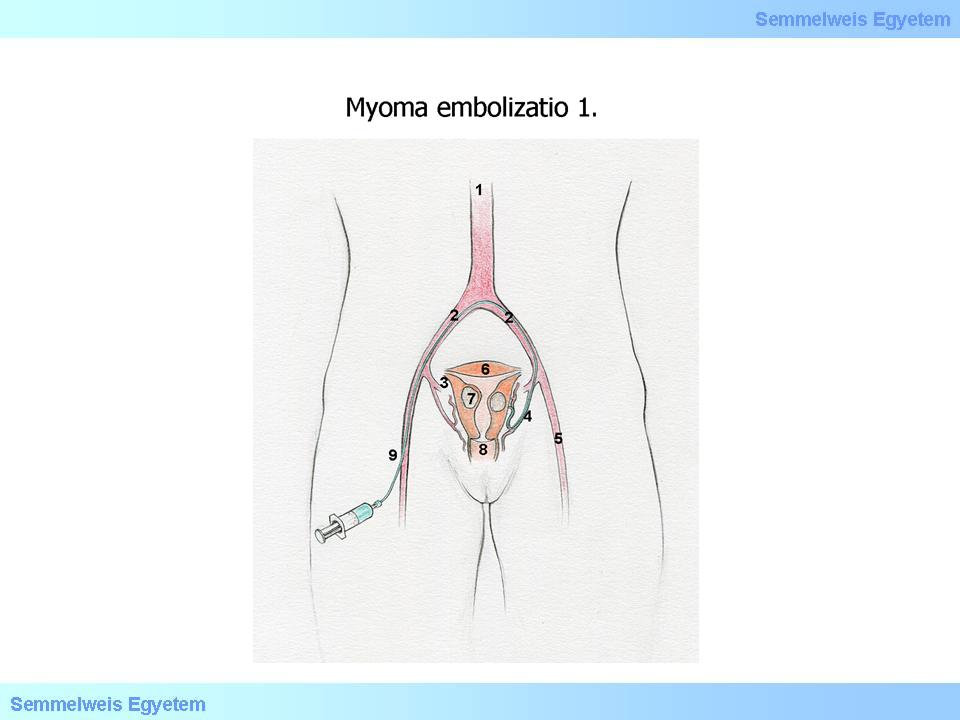
Illustration 1th: Embolization of the uterine artery I. (Kiss Balázs): (1) Aorta; (2) Arteria iliaca communis; (3) Arteria iliaca interna; (4) Arteria uterina; (5) Arteria iliaca externa; (6) Uterus; (7) Myoma uteri; (8) Vagina; (9) Arteria femoralis katéter
|
In case of gelatinized subserosal nodules this method is not applicable, since the loss of blood supply may result in cutting off the nodule entirely.
After successful surgery 80% of patients have a significant decrease in symptoms, increase of quality of life which persists for 3-5 years.
Of the more common complications post-embolization syndrome (25%), hematoma at the puncture site (15%), prolonged vaginal discharge (25%) and rejection of necrotic nodule (8%) and infection/septic necrosis (1-2%) is to be pointed out. In comparison to hysterectomy, inpatient care is significantly shorter (1-2 days), and the full recovery period is shorter too (1-2 weeks). In the longer term (3-7 years) due to recurrence of symptoms, 14-23% of the patients require further intervention and the majority chooses hysterectomy.
|

Please take a look at the picture!
|
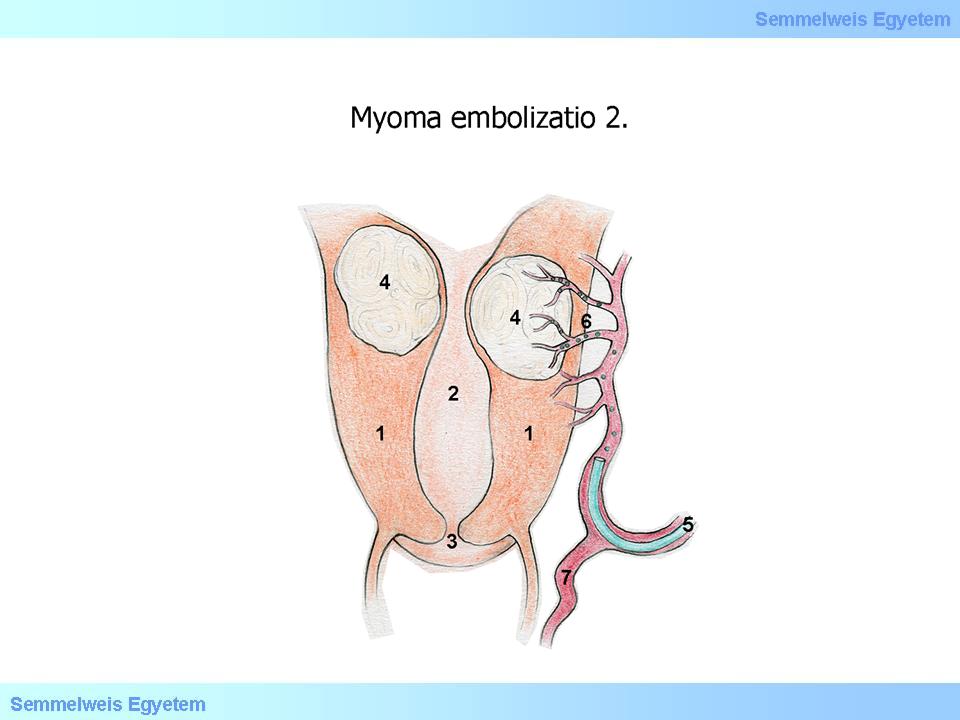
Illustration 2th: Embolization of the uterine artery II. (Kiss Balázs): (1)Corpus uteri; (2) Cavum uteri; (3) Cervix, canalis cervicis uteri; (4) Myoma uteri; (5) Arteria uterina katéter; (6) A tumor tápláló erek és embolizáló anyag; (7) Ramus vaginalis
|
MRI-guided focused ultrasound treatment (MRgFUS).
The latest non-invasive treatment method of uterus myomatosus gravis. The heat energy created with MRI-guided focused ultrasound causes coagulation necrosis which damages the tissue of the myoma nodule. The MRI technology guarantees the proper localization of the selected area, the control of ultrasonic waves and the control of temperature. There is no surgical wound, the patient is able to work 2-3 days after surgery. Similarly to the UAE, the treatment of gelatinized subserosal nodules is contraindicated. Another limitation is that only one node can be destroyed during a treatment session, and burn to the surrounding organs (e.g. bowel injury) can also occur. The widespread use of this method is limited by the fact that in some cases the procedure is very time consuming (up to 3 hours), and very expensive, and in some cases considerable pain occurs, which may last up to 2-3 weeks.
|

Please take a look at the picture!
|
Illustration 3th: MRI-guided focused ultrasound treatment – MRgFUS (Kiss Balázs)
|
|