| |
III./1.1.: Descriptive and functional anatomy of the stomach
III./1.1.1.: Introduction
|
 |
The stomach is a saccular dilation of the alimentary tract, situated in the continuation of the esophagus, below the diaphragm. It is responsible for digestion of food (protein breakdown), has an absorptive function and acts as a food reservoir as well (can expand up to 2-3 litres). Its strong muscle contractions transform the partially digested food into a viscous mass (chyme). The shape of the stomach - within certain limits - can be quite variable, depending on the build of the individual, the actual posture, the volume of gastric contents; most commonly hook or "J" shaped. The stomach is placed in the upper part of the abdominal cavity, in the epigastrium, and in the left hypochondrium. If we see it when empty, contracted, at first glance it is difficult to distinguish the stomach from the small intestines - in this case the peritoneal duplications attached to the lesser and greater curvatures (lesser omentum, greater omentum) help to make the right diagnosis.
III./1.1.2.: Gross anatomy
The parts of the stomach: gross inspection reveals the 4 main parts: next to the esophageal orifice (cardiac orifice), the cardia (gastric entrance) is situated. The name of the cardia refers to its close vicinity to the heart (Greek "kardia"); interestingly, the gastro-esophageal reflux disease (acidic regurgitation) causes a feeling described as "heartburn". Above and to the left from the cardia the gastric fundus is found, normally its upper part is filled with air. This detectable "gas bubble" is important during physical (percussion) and radiological diagnostics (chest X-ray, abdominal X-ray); the air, situated here - because of the buoyancy - helps to keep the stomach in its normal place.
The body (corpus) of the stomach is situated below the fundus; then it is followed by the pyloric part, containing the more dilated pyloric antrum which gradually gets narrower downwards and is continuous with the tube-like, narrow pyloric canal leading into the duodenum. The gastro-duodenal transition, as the gastric exit, has an important sphincter muscle - its thick ring is easily palpable on both the anatomical specimens and during surgery: the pyloric sphincter muscle regulates the movement of the gastric chymus (the gastric emptying).
At the empty, flattened stomach anterior and posterior surfaces can be distinguished, between them on the right side a concave lesser curvature, on the left side the convex greater curvature is found. The lesser curvature exhibits a sharp notch, the angular notch which indicates the border between the corpus and the pyloric part of the stomach. Between the greater curvature and the left edge of the esophagus another deep notch, the cardiac notch is located. The position of the greater curvature may be quite various, depending on the build of the individual, posture and the volume of gastric content, can descend to the L2-L5 vertebral level, these topographical differences can be visualised on contrast radiography (X-ray) images.
Two parts of the stomach can be considered topographically as more or less fix:
|
 |
-
- the most stable is the position of the cardia (at the level of the left side of Th11 vertebra), and
-
- the pylorus (in case of empty stomach at the level of L1 vertebra (this is the transpyloric plane), 2 cm right from the midline).
The anterior surface is mostly hidden by the liver (its left and quadrate lobes cover it), only the area between the lower margin of the liver and the left costal arch can be palpable through the anterior abdominal wall (Labbé's triangle): this area of the stomach can be reached easily during physical examination (palpation, percussion). The posterior surface of the stomach forms the anterior wall of the omental bursa (lesser sac= the space behind the stomach); more posteriorly the pancreas is located, covered by the posterior parietal peritoneum. The posterior aspect of the stomach contacts also the left kidney and adrenal gland.
The fundus of the stomach is situated below the left dome of the diaphragm and -on its left side- contacts the spleen. Below and behind the greater curvature the transverse colon is found. During pathological conditions, mostly in older age (in case of incomplete closure of the esophageal hiatus of the diaphragm, eg. due to muscle weakness) some parts of the stomach (eg. the fundus), due to the higher intra-abdominal pressure are protruded into the thoracic cavity (diaphragmatic hernia, hiatal hernia ). Congenital diaphragmatic hernia can be the result of developmental malformation of the diaphragm.
Another well known congenital malformation of the stomach is the hypertrophic pyloric stenosis: the thickening of the pyloric sphincter muscle narrows the pyloric lumen, thereby prevents gastric emptying. This problem causes very characteristic symptoms, eg. projectile vomiting of the newborn or few-week-old infant. The vomit contains no bile in this case. This disease can be characterized by the lack of relaxation of the pyloric sphincter. This motility problem is caused by the disturbed nitrergic (nitrogen monoxide, NO) transmission.
III./1.1.3.: The motility of the stomach
|
 |
The "proximal stomach" (cardia, fundus and upper part of corpus) has a reservoir function; during resting it is in tonic contraction. The distension caused by the food particles in the esophagus trigger the reflex relaxation of the stomach: receptive relaxation. The food, reaching the stomach creates adaptive relaxation of the stomach (accommodation). Both processes are based on vagal-effects (possibly the postganglionic nerve terminals release vasoactive intestinal polypeptide /VIP/ which reduces the smooth muscle tone of the stomach). The "distal stomach" (lower part of the corpus, pyloric antrum, pyloric canal) produces the gastric peristalsis by contraction of smooth muscle cells; that is fundamental in the mixing and emptying of the distal stomach.
The cooperation of the pyloric sphincter musculature is also necessary for the proper mixing function: the pyloric canal is open most of the time, but is rather narrow (about 1 mm in diameter). The antrum contraction causes only a few millilitres of gastric chyme entering into the duodenum, since then the pylorus closes completely. Then, at the closed pylorus retropulsion occurs: the movement of the gastric content turns back at the closed pylorus, resulting the ’grinding’ effect of the stomach. At that point, a question can be raised, whether how can the larger, indigestible objects (eg. bone pieces, swallowed ring) get through this narrow pyloric channel? Only during the so-called interdigestive phase can the total gastric emptying happen, in this case, due to the relaxation of pyloric sphincter muscle the bigger (above 1 mm in diameter) objects can be propelled into to the small intestine. Gastric emptying occurs during the relaxation of the pyloric sphincter muscle – in the mediation of this process nitric oxide (NO), VIP and PACAP (pituitary adenylate cyclase activating peptide) may play role.
At the cardia there is no anatomical sphincter muscle . But how can we explain the fact that -in a healthy person- the contractions of the stomach cannot press the gastric chymus back into the esophagus? The regurgitation into the esophagus is prevented by multiple factors, one of them is the tonic contraction of the smooth muscle of the lower esophageal sphincter (LES).
To inhibit the reflux, the normal anatomical situation is also required, where the cardia forms an acute angle with the esophageal opening (angle of His). This results that a valve-like portion of the cardia wall is able to close the cardiac orifice. To maintain this geometrical relation, the special course of smooth muscle of cardia and fundus is responsible, as well as the appropriate structure (both muscular and connective tissue) of the crura of the diaphragm. When the normally required His angle disappears, reflux can occur (gastroesophageal reflux disease, GERD). Similarly, in 2-3 month-old infants the not yet developed anatomical conditions (undeveloped His-angle) can allow the backflow of gastric chyme, resulting -in this case a physiological- reflux.
III./1.1.4.: Peritoneal relations of the stomach
|
 |
The stomach is completely covered by peritoneum, thus is a typical intraperitoneal organ (Fig. 9A-1.): the lesser curvature has a peritoneal duplicate extending from the liver (hepatogastric ligament ; together with its continuation, the hepatoduodenal ligament constitutes the lesser omentum). The peritoneal duplicates of the lesser omentum develop from the ventral mesogastrium . The bilayered hepatogastric ligament - which is situated practically in the coronal plane- reaches the lesser curvature of the stomach and there one peritoneal layer continues in front of the stomach while the other layer goes behind the stomach; these single peritoneal layers meet again at the greater curvature, forming again a duplicate called greater omentum (developmental derivative of the dorsal mesogastrium). This peritoneum duplicate hangs down from the greater curvature as an apron; reaching its lower end turns back, ascends again to form a four-layered membrane and attaches finally to the posterior abdominal wall.
Since the greater omentum is located in front of the transverse colon and the small intestines, when we look at the opened abdominal cavity, the very first structure we can see is this fatty peritoneal membrane, the greater omentum: one should lift it in order to see the small intestines situated behind. Between the stomach and the transverse colon the greater omentum fuses with the transverse mesocolon (which is the peritoneal duplicate of the transverse colon), thus makes the gastrocolic ligament (which, this way, is formed originally by the fusion of 6 layers of peritoneum).
The two peritoneal duplicates of the greater omentum are separate (ie. not fused) during the fetal age and in the first months after birth - so the omental bursa(peritoneal space behind the stomach) has a downward projection (omental or inferior recess) here, reaching the lower margin of the greater omentum. Later, however the peritoneal duplicates fuse together, closing this recess of the omental bursa.
The greater curvature sends another peritoneal duplicate toward the diaphragm: the gastrophrenic ligament; the spleen is situated in the lower part of this ligament, dividing it into two parts: the gastrosplenic and phrenicosplenic ligaments.
The intraperitoneal position of the stomach has important clinical consequences, eg. at the perforation of any origin (for example, leak can be made on the gastric wall due to ulcers or cancer) the gas (air) which filled the stomach gets into the peritoneal cavity. In this case, when gastric peroration is suspected, it can be diagnosed by percussion: the disappearance of liver dullness. Using radiological examinations, the presence of free abdominal air can also be detected at the highest point of the abdominal/peritoneal cavity (in upright patient between the liver and the diaphragm, in the hepatophrenic recess).
III./1.1.5.: Arterial blood supply of the stomach
|
 |
The arterial blood reaches the stomach from the branches of the celiac trunk (also called as tripus of Haller since it has three, almost equal-sized branches), arising from the abdominal aorta. Along the lesser and greater curvatures of the stomach anastomoses are created: at the lesser curvature the left gastric artery (direct branch of the celiac trunk) and the right gastric artery (the branch of the proper hepatic artery, sometimes arises from the common hepatic artery). Along the greater curvature (at approx. 1.5 cm from it) the left gastroepiploic/gastroomental artery (from the splenic artery) and the right gastroepiploic/gastroomental artery (from the gastroduodenal artery) make an arterial anastomosis which gives branches to supply the neighbouring areas of the stomach and also the greater omentum.
In addition, the area of the fundus of the stomach receives blood from the splenic artery - usually 4-5 separate branches (short gastric arteries), these vessels reach the stomach within the peritoneal duplication of the gastrosplenic ligament. The phrenicosplenic lig. includes the splenic artery; in the gastrosplenic lig. some branches of the splenic artery, the first part of the left gastroepiploic artery and the short gastric arteries are found.
The cardia area gets branches from the arteries of the esophagus (branches of the thoracic aorta) and from the inferior phrenic artery, which supplies the diaphragm.
Arteries supplying the stomach richly anastomose with each other; none of the gastric arteries is an end artery (Illustration 1.).
|

Observe the illustration!
|
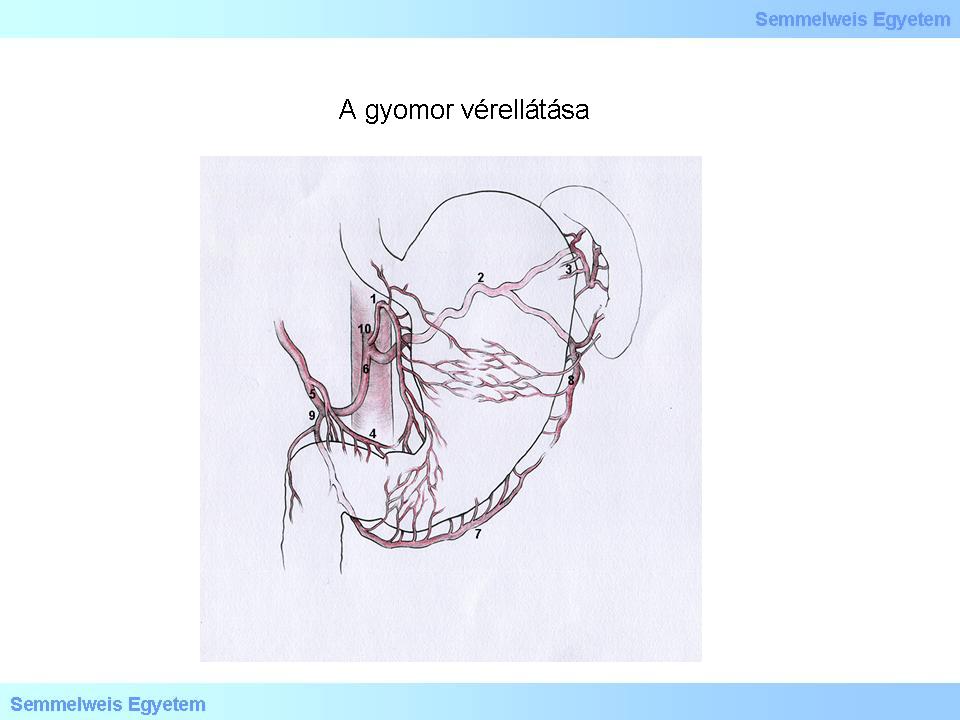
Illustration 1.: Arterial blood supply of the stomach
|
III./1.1.6.: Venous drainage of the stomach
The veins of the stomach run parallel with the arteries and empty into the portal vein system ; in addition to them separately should be mentioned the coronary vein of the stomach, which leads directly into the portal vein from the area of the lesser curvature. When discussing the venous drainage of the stomach, it is important to remember one of the so-called portocaval anastomoses (between the portal venous system and the superior vena cava area) found at the cardia region. The veins of the stomach course towards the portal vein, but the thoracic esophageal veins drain –through the azygos and the hemiazygos veins- into the superior vena cava system; these two venous systems have rich anastomosing connections at the esophagus-cardia border, below the mucous membrane.
This anastomosis at the cardia has practical significance when the portal venous circulation faces difficulties for some reason. In such cases (eg. at portal hypertension due to hepatic cirrhosis) increasingly larger amount of the intestinal venous blood flows towards the less resistance direction: through the gastric veins the blood gets into the veins around the cardia and then drains through the esophageal veins into the superior vena cava system. This increasing blood flow greatly dilates the lumen of the esophageal veins. In these patients, the esophageal submucosal veins are abnormally wide and fragile (esophageal varicosity); their wall ruptures easily, causing severe, often fatal bleedings.
III./1.1.7.: The lymphatic drainage of the stomach
The lymphatic vessels of the stomach run similarly to the veins; usually four major groups of lymph nodes and lymphatic drainage directions are described (Illustration 2.). The knowledge of them is important when searching for signs of the lymphogenic metastatisation of gastric tumors.
|

Observe the illustration!
|
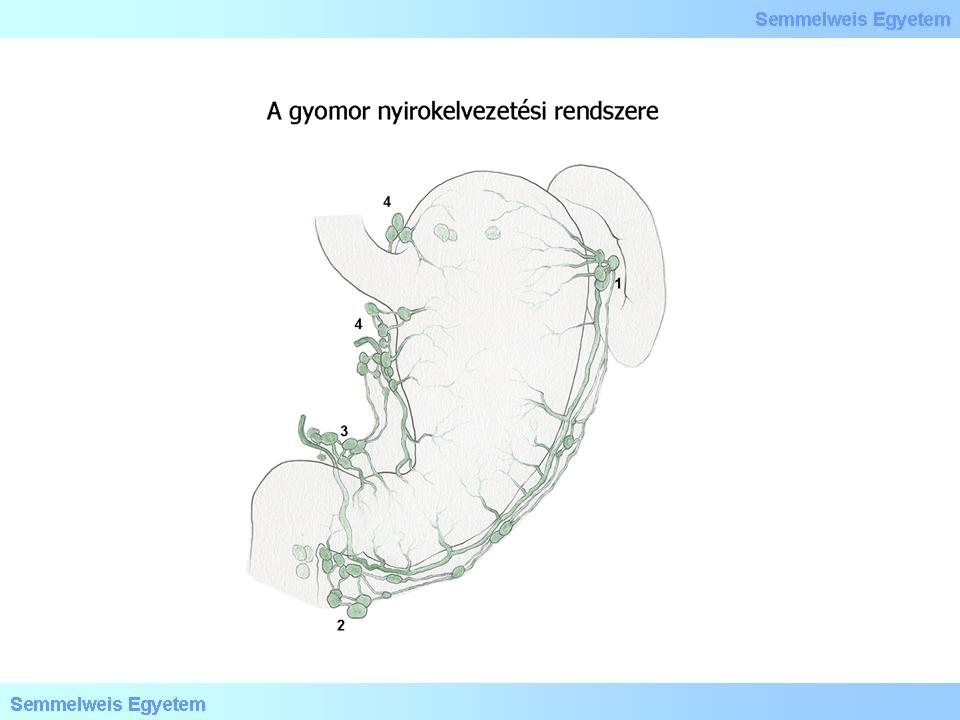
Illustration 2.: The main directions of the lymphatic drainage of the stomach
|
-
1) The area of the lesser curvature of the stomach and the fundus region: lymph vessels drain into the left gastric lymph nodes adjacent to the left gastric artery, from there lymph is directed either into the lymph nodes along the celiac trunk, and then into the cisterna chyli or –through the esophageal hiatus of the diaphragm- into the posterior mediastinal lymph nodes of the thoracic cavity.
-
2) The pancreaticosplenic lymph nodes are located at the splenic hilum; they receive lymph from the upper part of the greater curvature of the stomach and then forward the lymph to the cisterna chyli.
-
3) From the vicinity of the pylorus lymph gets into the pyloric lymph nodes.
-
4) From the right part of the greater curvature the right gastric lymph nodes take the lymph and also forward to the cisterna chyli.
Here we should also mention the left supraclavicular lymph nodes ("Virchow's nodes", located above the left clavicle), since the metastatic enlargement of these lymph nodes -preceding all other physical symptoms - can be an early sign of gastric cancer. The metastasizing cancer cells get here – although their course is not fully understood yet - probably through the lymphatics penetrating the esophageal hiatus and then running in the posterior mediastinum.
III./1.1.8.: Innervation of the stomach
|
 |
The extrinsic autonomic innervation of the stomach is provided by the vagus nerve and sympathetic fibers (Th6-8 spinal cord), the sensory fibers come from the dorsal root ganglia. The vagus nerves pierce the diaphragm through its esophageal hiatus (together with the esophagus) and the left vagus nerve (anterior vagal trunk) gives branches on the anterior aspect of the stomach, the right one (posterior vagal trunk) branches off to the posterior surface, their branches are anatomically and surgically preparable. The surgical transection of gastric branches of vagus nerve (selective vagotomy, proximal selective vagotomy) was recently an often used surgical treatment of gastric ulcer (a significant decrease of gastric acid secretion occured due to the loss of parasympathetic innervation). Nowadays the effective per os therapy is the key in reducing the acid secretion (Helicobacter pylori eradication treatment, proton pump inhibitors).
The preganglionic sympathetic fibers arise from the Th6-8 spinal segments (greater splanchnic nerve) and synapse in the celiac ganglion. From here, the postganglionic sympathetic fibers surround the arteries which supply the stomach (branches of the celiac trunk) and reach the stomach this way. The effect of the sympathetic nerves is mostly vascular (vasoconstriction).
Visceral afferent nerve fibers arise from the gastric mucosa, mediating visceral sensations (hunger) and pain. The visceral afferent fibers course together with the parasympathetic nerves, but the nociceptive fibers are found with the sympathetic nerves and this way they can reach the higher centres. The Head-zone of the stomach is found on the left side, corresponding to the dermatome of Th6-9 segment, at this skin area can the referred pain be felt in diseases of the stomach. Patients having peptic ulcer (a localized wound of the gastric mucosa, which penetrates through the lamina muscularis mucosae), can often point with one finger to the exact location of the pain: in the midline of the abdomen, at the epigastric region, above the navel.
The intrinsic nerve elements are parts of the enteric nervous system (ENS): the nerve cells and nerve fibers of the submucosal plexus (of Meissner) are found in the tela submucosa; the myenteric plexus (of Auerbach) is located between the circular and longitudinal muscle layers. These plexus neurons can receive the parasympathetic preganglionic fibers, which synapse here (the postganglionic neurons innervate the smooth muscle cells and glands, the mucosa and also the immune cells) but can also act as afferent, efferent and interneurons of local, gastrointestinal reflexes (gastro-entero-colic reflexes). The gastric smooth muscle is mainly regulated by the local nerve plexuses.
III./1.1.9.: Interstitial cells of Cajal
|
 |
More than a hundred years ago Ramon y Cajal described the intestinal interstitial cells, which were later named after him. Cajal characterized these cells as primitive "interstitial neurons" placed between the autonomic nerve endings and smooth muscle cells. During light microscopy, these cells were seen having processes (branching cytoplasm) and heterochromatic nuclei. The interstitial cells form a complex network around nerve plexuses and smooth muscle cells.
According to our present knowledge, these cells have non-neuronal origin (ie. not neurons or glial cells), but are derived from mesenchyme: modified smooth muscle cells which have lost their contractility. The interstitial cells occur in all parts of the gastrointestinal tract. Their common fine structural characteristics: they show mainly "mioid" (ie. similar to the visceral smooth muscle cells) features: basal lamina, caveolae, focal densities (elementary sarcomeres, dense bodies), an extensive endoplasmic reticulum, numerous mitochondria and intermediate filaments are found in them. Some types have structural characteristics resembling to fibroblasts also: well developed secretory apparatus, especially moderately dilated cisterns of the rER, long and branching cytoplasmic processes. Synapse-like contacts with the nerve endings could be demonstrated and also very close appositions or gap junctions with the smooth muscle cells were detected.
One group of the Cajal cells has a key role in mediating the inhibitory enteral innervation (neurotransmission) while the other subpopulation acts as intestinal pacemaker cells (basal electrical rhythm, "slow wave" generators). The Cajal cells of the submuscular plexus (found at the inner side of the inner, circular muscle layer, facing the tela submucosa) were observed to have both of these functions. It has been shown that the interstitial cells of Cajal are able to express the proto-oncogene KIT and its protein product (c-kit receptor, membrane receptor tyrosine kinase). The safest method to identify Cajal cells is the combined demonstration of their electrone microscopic characteristics and the c-Kit positivity. Their role in the development of gastrointestinal stromal tumors (GIST) is currently a subject of extensive research.
III./1.1.10.: Internal relief of gastric mucosa
As seen in an empty stomach (when opened or during endoscopy) there is a well defined, strong longitudinal fold system (gastric folds, gastric rugae); these lengthwise folds run mainly parallel with the lesser curvature, coursing from the cardia to the pylorus (the "gastric pathway" or "Magenstraße" in German). Here, fluids have almost a direct route from the cardia to the pylorus.
|
 |
The rest of the stomach, particularly the fundus contains an irregular network of mucosal protrusions, forming compartments to accommodate larger food particles (Figure 3.). When having a closer look at the mucosal surface (and especially using magnifying glass/loupe magnification), a system of fine processes (areolae gastricae), among them funnel-like depressions (gastric pits, foveolae gastricae) can be recognized. The tubular glands of the stomach open into these pits. The esophagus-cardia border is clearly visible on the mucous membrane during endoscopic examination; on well-fixed specimens can also be detected with the naked eye. In this area the stratified squamous, non-keratinized epithelium of the esophagus abruptly changes into the simple columnar epithelium of the stomach.
|
|