 |
IV./1.1.: Histological structure
IV./1.1.1.: General features
A pear-shaped hollow organ of muscular wall, the uterus is composed largely by myometrium made up of smooth muscle, and lined by a mucous membrane (endometrium). The external covering of the organ is termed perimetrium (Photo 1).
|

Study the photo!
|
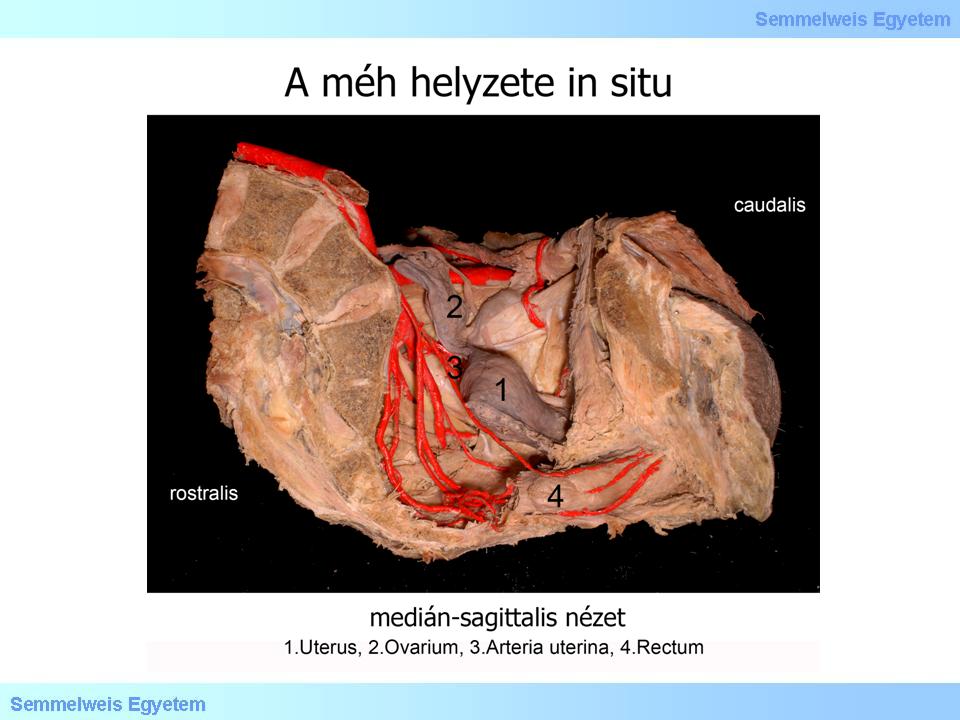
Photo 1: Uterus in situ – Attila Molnár, and Attila Balogh
|
IV./1.1.2.: Endometrium
The epithelium of endometrium in the fundus and corpus is single columnar, also containing groups of ciliated epithelial cells. The cervix contains fewer ciliated cells, the columnar cells being taller, their nuclei are closer to the base. Secretory granules containing mucin occur in the apical cytoplasm.
|
 |
The tunica propria of the endometrium contains abundant connective tissue cells, reticulin fibres and a large amount of amorphous intercellular substance. Spindle-shaped cells of the stroma, resembling of mesenchyme, are small, with ovoidal nuclei. These cells constitute what is called spinocellular connective tissue. Lymphocytes and other types of white blood cells frequently occur among the cells of connective tissue. The stroma of the cervix is more compact, with more fibres and fewer cells. The endometrium of the cervix is thrown up into folds resembling palm leaves (plicae palmatae).
The tunica propria of fundus and corpus contains simple tubular glands spanning the entire width of endometrium. Terminal parts of these glands often bifurcate and extend into the innermost layer of myometrium. The epithelium of the glands is similar to that of the surface but with fewer ciliated cells. The glands of the cervix contain tall epithelial cells, like those of the surface epithelium. Profusely branching, these glands belong to the compound tubular type, and they show only moderate changes of morphology during the menstrual cycle. However, the composition of their secretion undergoes considerable transformation under the effect of the hormones regulating cyclic changes. The glands proliferate during pregnancy, and their secretion is also increased.
|
 |
Based on its composition and changes during the menstrual cycle, the endometrium can be divided into two layers. One is a narrow strip called stratum basale, adjacent to the myometrium, which does not participate in cyclic mucosal alterations. The other layer above it, termed stratum functionale, is the site of cyclic changes. The stratum functionale, whose thickness and structure undergo marked alterations during the cycle, can be further subdivided into two sublayers. The narrow zone beneath the surface epithelium is more compact due to a very large number of connective tissue cells. This is called stratum compactum, which contains the straight, cervical portions of the glands. The next zone below it, termed stratum spongiosum, appears spongy owing to the convoluted and distended portions of the mucosal glands.
Blood supply of the mucosa comes from the myometrium via two arteries. One group of short and straight arteries supply the stratum basale. The other group of longer helical arteries maintain vascular supply of the stratum functionale. The helical arteries form a network of distended vessels (lacunae) at the border between the stratum compactum and stratum spongiosum, near to the surface of the mucosa. Hormonal sensitivity of the smooth muscle cells of the two arterial types is different. The thin-walled veins of endometrium form a network. Drainage of endometrium occurs via the venous network of myometrium. Lymph vessels build profuse plexuses in the endometrium, myometrium and perimetrium, however, they are absent from the superficial layer of the endometrium.
During the reproductive period of life, i.e. in the course of 30-35 years elapsing between the menarche and the menopause, the mucosa of the uterus undergoes cyclic changes, with the exception of the cervix. First, the thickness of mucosa is enhanced, and then it is decreased, finally leading to destruction and desquamation of the superficial layer (stratum functionale). Duration of the cycle ranges from 21 to 35 days, on average 28 days, in the course of which the histological structure of mucosa changes by the day. This process is subdivided into histological periods, albeit without sharply defined borders.
|
|